INTRODUCTIONTraumatic bone cysts may be characterized by the presence of an asymptomatic cavity in bone with no epithelial lining. Traumatic bone cysts were described in 1929;1 they are commonly found in the metaphysis of long bones, but are rare in the jaws2.
Traumatic bone cysts may be classified as unicameral3, simple4, solitary5, hemorrhagic6, or idiopathic7. They are usually asymptomatic and appear on routine radiographies. Because of a lack of unique clinical and radiographic features, it is important to establish the differential diagnosis between traumatic bone cysts and other bone lesions of the jaws - especially translucent lesions. The purpose of this study was to describe the clinical, surgical, and radiographic features of traumatic bone cysts that were diagnosed at an oral pathology center during a 15-year period.
MATERIAL AND METHODSA retrospective study was made of patients that had been diagnosed with traumatic bone cysts at an oral pathology center from 1992 to 2007. Two previously trained researchers reviewed the surgical reports in patient registries, panoramic radiographs, and hematoxylin-eosin stained slides to gather the following data:
(1) Clinical data: sex, age, pain, history of local trauma, anatomical site, presence of an enlarged mass;
(2) Radiographic data: number of lesions, whether locular, and diameter;
(3) Surgical: content of the pathologic cavity, and treatment.
Data were tabulated using the Bioestat 5.0 statistical package. Descriptive statistics were applied to obtain central tendency and dispersions measures. The institutional review board approved the study (protocol nº. 085/07.
RESULTSThere were 26 cases of traumatic bone cysts were diagnosed in the 15-year period, comprising 0.58% of the total number of histopathology reports, and 13.5% of the bone lesions related to odontogenic tumors (Table 1). Table 2 summarizes the clinical, radiographic, and surgical findings of these traumatic bone cysts.
Clinical findingsOf 26 patients, 17 (65.4%) were male and nine were female (34.6%). The age ranged from 10 to 70 years; the mean was 19.5 years and the median was 16 years (Q1 = 15; Q3 = 20). Most cases were asymptomatic (88.5%); there was a history of trauma in only four patients (15.4%). All of the cases were on the mandible - 18 (69.2%) in the posterior area and eight (30.8%) in the anterior region. There was an enlarged mass in three cases (11.5%).
Radiographic findingsThe lesions were solitary in most cases (96.1%); 19 (73.1%) were unilocular (Figure 1A). Seven cases were multilocular (26.9%), which gives the lesion the appearance of a tumor. The diameter on panoramic radiographs ranged from 1.5 to 8 cm; the median was 3.5 cm.
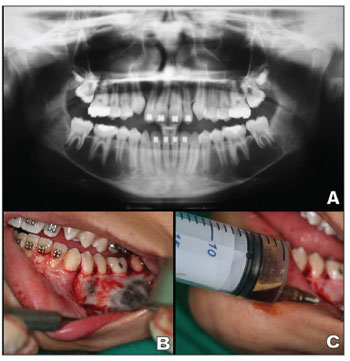
Figure 1. A: Panoramic radiograph showing a bilateral multilocular lesion with scalloping along the roots of teeth in the posterior area of the mandible. B: Intraoral view after making a mucoperiosteal flap to show bone expansion with hemorrhage. C: Aspiration biopsy showing serous-bloody fluid.
During surgery (Figure 1B), air was noted within the pathologic cavity in 18 cases (69.2%). There was serous-bloody fluid in five cases (19.2%) (Figure 1C) and serous fluid in three cases (11.6%). The treatment in all cases consisted of surgery to explore the cavity and curettage of the bone walls.
DISCUSSIONTraumatic bone cysts are rare lesions of the jaws. They are classified by the World Health Organization8 as part of a group of bone lesions that include the ossifying fibroma, fibrous dysplasia of bone,
central giant cell lesions, aneurismatic bone cysts, and cherubism. Although traumatic bone cysts were described at the beginning of the 20th century, the pathogenesis remains unclear and speculative. The most accepted version at present is the traumatic-hemorrhagic theory, which suggests that lesions develop if intramedullary clots due to trauma do not undergo lysis or resolution9. This theory explains why traumatic bone cysts occur more often in young individuals (an age at which trauma occurs more often) and also explain the presence of blood within the cavity at the time of surgical exploration. Reports of trauma at the site of lesions and the presence of blood in the cavities, however, are uncommon, as seen in our sample. This opens the possibility that microtrauma of teeth and the alveolar ridge are involved in the pathogenesis of traumatic bone cysts10.
According to several authors, most cases of traumatic bone cysts present in young patients, although they may be detected at any age11-13; our findings were similar - there was a preference for the first two decades of life. MacDonald-Jankowski12 has stated that a reduced prevalence of traumatic bone cysts in older patients suggests that this lesion may be self-repairing - we believe this explanation is merely speculative. A few studies have reported no sex preference13,14, but males predominated in our series. Zehetgruber et al.15 have reported a similar prevalence for extrafacial variants in young patients.
Traumatic bone cysts are considered almost exclusively mandibular lesions, with a preference for the posterior areas (body and ramus) - although the symphysis may also be a site16,17. They rarely may be present in the maxilla18, although some studies have found a 25% incidence of cases in this bone19. Possibly its almost exclusive location in the mandible is related to its pathogenesis; the trauma-hemorrhage theory may be an explanation because the mandible, which has more cortical bone, repairs itself more slowly compared to the maxilla.
Most cases of maxillofacial traumatic bone cysts are asymptomatic and do not cause expansion of the cortical area - these cysts are diagnosed as accidental findings in routine radiographs10,12,18,20. Except for three symptomatic cases in our series, all other were discovered in panoramic radiographs for conventional dental treatment, such as removal of third molars and orthodontic therapy. There was no bone expansion in about 92% of cases, which reflects the potential that this lesion has for developing in medullary spaces.
Traumatic bone cysts generally show up as unilocular radiolucent areas in the posterior portion of the mandible; its margins are scalloped among dental roots9-11 (Figure 2). This radiographic pattern, however, may vary - the cyst may be multilocular, associated with unerupted/impacted teeth, and several cysts may be present in the same patient17 (Figure 3). Therefore, traumatic bone cysts should be part of the differential diagnosis of maxillary radiolucent lesions - together with dentigerous cysts, keratocystic odontogenic tumors, ameloblastomas, odontogenic myxomas, aneurismatic bone cysts, focal osteoporotic bone marrow defect, intraosseous vascular malformations, central giant cell lesions, among others. Although we found no association with unerupted/impacted teeth in our sample, the keratocystic odontogenic tumor and the ameloblastoma were the most frequently mentioned tumors in the initial diagnosis, especially when the radiographic image showed a multilocular cyst.
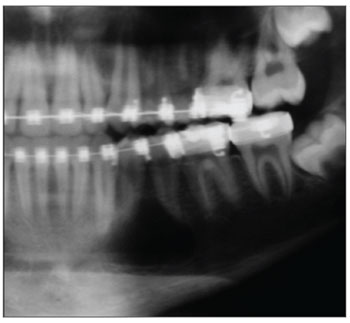
Figure 2. Panoramic radiograph showing a translucent unilocular image in the body of the left mandible. Radiotransparency reveals the classical scalloping around premolar apices.

Figure 3. Multilocular traumatic bone cyst in the body of the left mandible; this image first suggested a tumor. The cortical plate is preserved.
A few authors have reported the occurrence of multiple traumatic bone cysts and their association with fibrous/bony lesions - such as the florid cemento-osseous dysplasia - especially in older patients20-23. Wakasa et al.23 have suggested that the florid cement-osseous dysplasia may precede traumatic bone cysts when these two conditions are associated, which suggests that disordered production of trabeculae in the former may obstruct lymphatic drainage and induce traumatic bone cyst formation. Our single bilateral case was not associated with other disorders - this patient was aged 10 years (Figures 1A, 1B, 1C).
The histology of traumatic bone cysts reveals only a connective tissue membrane lining the pathologic cavity, characteristic of pseudocysts. Cholesterol crystals, hemorrhagic foci, and osteoclasts may be found10,23,24. A final diagnosis of a traumatic bone cyst is almost invariably made at the time of surgery; the material available for histology is usually sparse because of the difficulty in removing the thin connective tissue membrane. Surgeons usually encounter an empty cavity, although there may be blood, serum, or both. Kuhmichel & Bouloux20 have noted that such content in the bone cavity may represent different stages in the development of traumatic bone cysts; we also believe this hypothesis is speculative.
The treatment of choice for traumatic bone cysts is surgery for curettage of the bone walls, which generally results in short-term healing10,18,24,25. Recurrences are rare, and usually occur within three months of surgery. Cases of multiple cysts or those associated with florid cemento-osseous dysplasia have high recurrence rates - respectively about 71% and 75%26.
CONCLUSIONIn summary, although we found a predominance of traumatic bone cysts in males, the clinical and surgical findings in our sample concurred with other published studies. A higher prevalence of cases in the mandible and in young individuals, infrequent histories of trauma, and a paucity of lesions with serous-bloody content reflect a need to debate the true pathogenesis of traumatic bone cysts. In radiographs, the multilocular pattern comprises about one third of cases, and may simulate tumors in the jaws.
REFERENCES1. Lucas CD, Blum T. Do all cysts in the jaws originate from the dental system? J Am Dent Assoc. 1929;16:647-61.
2. Saito Y, Hoshina Y, Nagamine T, Nakajima T, Suzuki M, Hayashi T. Simple bone cyst. A clinical and histopathologic study of fifteen cases. Oral Surg Oral Med Oral Pathol. 1992;74(4):487-91.
3. Jaffe H, Lichtenstein L. Solitary unicameral bone cyst. Arch Surg. 1942;44:1004-25.
4. Kuroi M. Simple bone cyst of the jaw: Review of the literature and report case. J Oral Sur. 1980;38(6):456-9.
5. Rushton MA. Solitary bone cysts in the mandible. Br Dent J. 1946;81(2):37-49.
6. Fickling BW. Haemorrhagic bone cyst. Proc R Soc Med. 1955;48(11):988-9.
7. Jones AC, Baughman RA. Multiple idiopathic mandibular bone cysts in a patient with osteogenesis imperfecta. Oral Surg Oral Med Oral Pathol. 1993;75(3):333-7.
8. Barnes L, Eveson JW, Reichart P, Sidransky D. WHO classification of tumours: head and neck tumours. Lyon: IARC Press; 2005.
9. Howe GL. "Haemorrhagic cysts" of the mandible. I. Br J Oral Surg. 1965;3(1):55-76.
10. Harnet JC, Lombardi T, Klewansky P, Rieger J, Tempe MH, Clavert JM. Solitary bone cyst of the jaws: a review of the etiopathogenic hypotheses. J Oral Maxillofac Surg. 2008;66(11):2345-8.
11. Forssell K, Forssell H, Happonen RP, Neva M. Simple bone cyst: review of the literature and analysis of 23 cases. Int J Oral Maxillofac Surg. 1988;17(1):21-4.
12. MacDonald-Jankowski DS. Traumatic bone cysts in the jaws of a Hong Kong Chinese population. Clin Radiol. 1995;50(11):787-91.
13. Perdigão PF, Silva EC, Sakurai E, Soares de Araújo N, Gomez RS. Idiopathic bone cavity: a clinical, radiographic, and histological study. Br J Oral Maxillofac Surg. 2003;41(6):407-9.
14. Kaugars GE, Cale AE. Traumatic bone cyst. Oral Surg Oral Med Oral Pathol. 1987;63(3):318-24.
15. Zehetgruber H, Bittner B, Gruber D, Krepler P, Trieb K, Kotz R, et al. Prevalence of aneurysmal and solitary bone cysts in young patients. Clin Orthop Relat Res. 2005;439:136-43.
16. Sapp JP, Stark ML. Self-healing traumatic bone cysts. Oral Surg Oral Med Oral Pathol. 1990;69(5):597-602.
17. Tong AC, Ng IO, Yan BS. Variations in clinical presentations of the simple bone cyst: report of cases. J Oral Maxillofac Surg. 2003;61(12):1487-91.
18. Peñarrocha-Diago M, Sanchis-Bielsa JM, Bonet-Marco J, Minguez-Sanz JM. Surgical treatment and follow-up of solitary bone cyst of the mandible: a report of seven cases. Br J Oral Maxillofac Surg. 2001;39(3):221-3.
19. Matsumura S, Murakami S, Kakimoto N, Furukawa S, Kishino M, Ishida T, et al. Histopathologic and radiographic findings of the simple bone cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(5):619-25.
20. Kuhmichel A, Bouloux GF. Multifocal traumatic bone cysts: case report and current thoughts on etiology. J Oral Maxillofac Surg. 2010;68(1):208-12.
21. Horner K, Forman GH. Atypical simple bone cysts of the jaws. II: A possible association with benign fibro-osseous (cemental) lesions of the jaws. Clin Radiol. 1988;39(1):59-63.
22. Mahomed F, Altini M, Meer S, Coleman H. Cemento-osseous dysplasia with simple bone cysts. J Oral Maxillofac Surg. 2005;63(10):1549-54.
23. Wakasa T, Kawai N, Aiga H, Kishi K. Management of florid cemento-osseous dysplasia of the mandible producing solitary bone cyst: report of a case. J Oral Maxillofac Surg. 2002;60(7):832-5.
24. Baqain ZH, Jayakrishnan A, Farthing PM, Hardee P. Recurrence of a solitary bone cyst of the mandible: case report. Br J Oral Maxillofac Surg. 2005;43(4):333-5.
25. Shigematsu H, Fujita K, Watanabe K. Atypical simple bone cyst of the mandible. A case report. Int J Oral Maxillofac Surg. 1994;23(5):298-9.
26. Suei Y, Taguchi A, Tanimoto K. Simple bone cyst of the jaws: evaluation of treatment outcome by review of 132 cases. J Oral Maxillofac Surg. 2007;65(5):918-23.
1. Master's degree in health science, Nucleus for Graduate Studies in Medicine, Federal University of Sergipe (NPGME/UFS) (Doctoral student in health science, NPGME/UFS).
2. Master's degree in oral and maxillofacial surgery and trauma, Dentistry School of Pernambuco (FOP/UPE) (Doctoral student in oral and maxillofacial surgery, Dentistry School of Ribeirao Preto - FORP/USP).
3. Dental surgeon, trained at the Dentistry School of Pernambuco (FOP/UPE) (Dental surgeon).
4. Master's degree in oral and maxillofacial surgery and trauma, Federal University of Rio de Janeiro (UFRJ) (Coordinator of the oral surgery course, Center for Further Studies, Sergipe (CAP-SE)).
5. Doctoral degree in oral pathology, Federal University of Rio Grande do Norte (UFRN) (Professor of oral pathology, Dentistry School of Pernambuco - FOP/UPE).
6. Doctoral degree in oral and maxillofacial surgery and trauma, Dentistry School of Pernambuco (FOP/UPE) (Professor in the Dentistry Department and the NPGME/UFS).
Faculdade de Odontologia de Pernambuco (FOP/UPE) - Dentistry School of Pernambuco. Universidade Federal de Sergipe (UFS) - Federal University of Sergipe.
Send correspondence to:
Universidade Federal de Sergipe, Campus da Saúde, Departamento de Odontologia
Rua Cláudio Batista, s/n. Bairro: Sanatório
CEP: 49060-100. Aracaju, SE, Brazil
Email: saqmartins@hotmail.com
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on January 25, 2011.
Accepted on November 24, 2011. cod. 7540.


