INTRODUCTIONThree swallowing patterns have been described: visceral, somatic and irregular. Visceral is the swallowing at birth, also known as infantile swallowing. The tongue is relatively large in newborns and placed more anteriorly, between the anterior gum rollers and it aids in anterior lip sealing1-5. With the eruption of the first deciduous teeth, the suction push reduces and is slowly replaced by the push to bite and, at this stage; deglutition is called irregular1,2. Although deglutition is the first function established in the stomatognathic system, it is the last process to mature, because as bone structures are under growth and dentition is still not installed, the tongue cannot acquire mature posture and movement. It is only when the child is about two years of age, a transitional (irregular) deglutition pattern is expected for the mature pattern, with the tongue within the confines of the teeth arches, with the soft tissue better adjusted and the lips sealed, called somatic deglutition6-8.
Mixed dentition stage is a phase of development in which there are numerous changes to the stomatognathic system, and studies say that it is at this stage that there should be the definitive transition from the infantile deglutition pattern (visceral) to the mature pattern (somatic). For a number of reasons which are still incompletely explained, "infantile deglutition" may continue to beyond the replacement of the deciduous teeth, being classified as atypical deglutition3,5,8. Atypical deglutition has been attributed to suction without nutritional purposes, use of bottles, oral breathing, central nervous system disorders and anatomical changes5-9. Notwithstanding, there is no consensus regarding its etiology.
Studies have shown that deglutition is an activity which is coordinated together with other oral functions, and it requires a straight interaction between different muscle groups. In order to synchronize suction and swallowing, it is necessary to have a very close relationship between the muscles in the oral region in the generation of suction pressure - to open and close the mouth, and the tongue in order to form the bolus and its peristaltic transportation to the pharynx10. During oral feeding, respiratory mechanics involves the proper activation of the diaphragm, intercostal muscles and the upper airway muscles - from the nose to the glottis10. Recent studies have reported that adenoid and palatine tonsil hyperplasia is the second most frequent cause of upper airway obstruction and, consequently, oral breathing in children11-15. The relationship between oral breathing and atypical deglutition has already been studied16-20, but it is still controversial21. One recent study22 assessed the oropharyngeal distance in teleradiography made in the orthostatic position; nonetheless, it did not detect differences between the groups studied and in the different age ranges evaluated. Therefore, the goal of the present study was to compare the oropharyngeal distances in teleradiographies, taken in natural head position of children in physiologically mixed dentition stage, with atypical deglutition and normal deglutition.
MATERIALS AND METHODSIn this retrospective, analytical and observational cross-sectional cohort, we assessed side-view teleradiographies from children of both genders, in mixed physiological dentition, between 7 and 11 years of age1-3,5, treated in the functional orthopedics of maxillae program of the Systemic Dentistry Society of São Paulo Clinic. All side-view teleradiographies selected had the following characteristics: 18x24 cm, taken with a Siemens device, for 1 second, 6 Kvp and 1.5 meters of focal distance, carried out with the patient under natural head position. After selecting the side-view teleradiographies, we carried out a cephalometric exam in a dark room, using a radiologic view box, overlapping an acetate sheet over the teleradiography. We outlined the anatomo-radiographic structures of the PAS variable, also called lower airway: pharyngeal width where, radiographically, the posterior tongue border crosses the lower mandible border, all the way to the point nearest the posterior pharyngeal wall20,23(Figure 1).

Figure 1. PAS (lower airway) Cephalometric value: pharynx width at the point where, radiographically, the posterior tongue border crosses the inferior mandible border, all the way to the closest point to the posterior pharyngeal wall.
Side-view radiographs without good visibility of anatomical structures used in the cephalograms were taken off the sample. Patients with dental agenesis; congenital orofacial malformations; orthodontic, functional orthopedic and orofacial myofunctional treatments prior to the study, doubts or inaccuracies as to the swallowing diagnosis were taken off the study. In order to define the control and experimental groups, we used the labial opening pressure test with saliva swallowing2,3, carried out by three functional orthopedists/orthodontists simultaneously, settling, by consensus, to which group the child's teleradiography would belong to:
- Normal deglutition (control group): labial sealing and positioning the tongue tip on the papila21;
- Atypical deglutition (experimental group): atypical labial pressure, tongue pressure against the anterior teeth or between the dental arches21.
We selected 20 side-view teleradiographies from 20 patients diagnosed with atypical swallowing and 20 side-view teleradiographies from 20 subjects clinically diagnosed with normal swallowing. With these teleradiographies, we carried out a pilot study in order to calculate the size of the sample: we calculated the control group's standard deviation and the difference between the mean values from the control and experimental groups; with a significance level of 0.05 and test power of 0.10, we obtained the desired sample size of 110 teleradiographies, 55 in each group. After we calculated the sample size, we selected the sample based on the same criteria of the pilot study aforementioned.
The side-view teleradiographies of the study and control groups were randomly classified and numbered in a sequence. This procedure was carried out so that the examiner, who did the measurements manually, would be blind as to which group the teleradiography belong to, thus avoiding biases. The numbered teleradiographies were handed over to the examiner in order to carry out the aforementioned standardized measures, writing them down in the data collection tool. In order to minimize systematic error, the same examiner collected the data from the entire sample at two occasions, within a 20-day interval between them.
After measuring and writing down the data corresponding to all the radiographs, information regarding age, gender and the presence or absence of atypical deglutition was added. In order to compare the variables between the two groups, we used the Mann-Whitney, test, finding the mean, median, minimum median, maximum median, standard deviation and the test values assessing data significance. In order to control variables age and gender, we carried out a covariance analysis (ancova). In order to check for intra-examiner consistence, we employed the Wilcoxon test for related samples, on a possible difference of measures at the two data collection times. The significance level used for the statistical tests was 5%.
Because this is a retrospective study using side-view teleradiographies from patients who have been already treated, and also because this study did not do experiments with human beings, it did not require an informed consent form, making sure that all necessary measures were taken in order to maintain the confidentiality of the information given by the patients. Only the patients initials were written down into the collection device, and there was no way that any other person, except for the researcher, could identify to whom each teleradiography belonged. The study protocol for this study was previously approved, without restrictions, by the Ethics in Research Committee of the Institution.
RESULTSThis study's sample involved 110 side-view teleradiographies, belonging to 52 female patients and 58 males, and such gender difference was not significant (
p=0.1266). The mean age of the control group (normal deglutition) was 9.46 years (standard deviation = 1.83) and 10.05 years in the experimental group (standard deviation = 2.13), without significant difference (
p=0.6345).
In order to compare the values between the two groups we used the Mann-Whitney test. The median width of the PAS variable was 7 mm, in the experimental group and 10 mm in the control group (Table 1 and Figure 2), with a statistically significant difference (
p <0.001). This significance was maintained after employing the covariance analysis (ancova) in order to control the age and gender variables in the samples. To assess intra-examiner uniformity, we employed the Wilcoxon test for selected samples on the possible difference of the measures at the two data collection occasions, and we did not find statistically significant differences concerning this possible difference (
p=0.989).
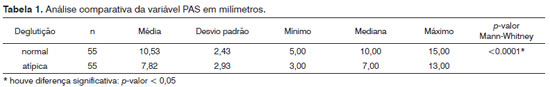
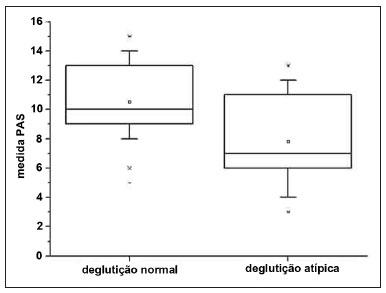
Figure 2. Set of PAS value data from the normal and atypical deglutition groups. The inner line of the box outlines the data set median value.
This study's results showed a significant difference in the PAS radiographic measure between the groups studied. The value found (10mm median) in the control group is very similar to the value indicating normality20. The age at which a child reaches the mature deglutition standard is controversial in the literature, varying between 18 months and 6 years of age21. Therefore, we chose to collect the data from children at the age of mixed physiological dentition (between 7 and 11 years)1,3-5.
Although the age range investigated is broad, the results from this study did not show statistical differences between groups with regards to age of the subjects. Still, assuming that age and gender could be variables which could increase or decrease of the value studied, we analyzed the covariance (ANCOVA) in order to control age and gender variables. This threshold showed that there still is a significant difference (
p<0.001) between the two groups for the PAS variable, regardless of age and gender.
One study21 associates atypical deglutition and occlusal problems in oral breathing children and did not find a statistically significant correlation between atypical deglutition and anterior open bite in 8 to 12 year-old oral breathers. The authors also stated that dental occlusion is not responsible for these children having inadequate deglutition, it is rather associated with the open mouth posture they have in order to keep the air flow and/or because of a hyperplastic palatine tonsil. We believe that the results from the present study may support such hypothesis, since the airway reduction, very likely caused by tonsil hyperplasia, would trigger the oral breather syndrome, change in tongue posture and, consequently, causing atypical deglutition.
PAS has been described as the distance between the back of the pharynx to the front, where the tongue base is20. We believe that factors such as age and gender are perhaps less important than the posture of the tongue in the allocation of the PAS variable radiographic value. Perhaps, it is the tongue posture that defines this distance, and not the airway lumen itself.
Ceylan & Oktay10 noticed that the radiographic anatomy of the pharyngeal space is related to the mandibular position. We believe that the lowered tongue may be able to keep the mandible in a posterior position and trigger distal occlusion, a frequent type of malocclusion in oral breathers22.
Vieira & Villela22 performed cephalometric studies evaluating oropharyngeal distance values in atypical swallowing in different age groups in radiographies taken in the standing position. A difference of the present study is the use of teleradiographies taken with the patient in natural head position. We believe that the change in head tilt in the radiograph taken with the patient standing, may change the airway measurement; nonetheless, further studies are needed in order to assess this issue. However, as for the age data, the results of this study agree with the findings from Vieira & Villela21, because the value studied did not vary with age.
We collected data from the entire sample at two times in an attempt to minimize a systematic error. We checked to see whether the data collected by the same examiner at two different occasions could vary significantly. This was not the case - proving an intra-examiner consistency. Although the variables are measurable, we used a nonparametric statistical test, due to abnormal sample data distribution. Since this study was retrospective, based on teleradiography analyses, one limitation was that it was not possible to assess whether the distance measured can be changed after correction of the swallowing movement disorder. Further studies should be conducted to evaluate this hypothesis.
Despite the focus given to the dental study, we believe that this is a multidisciplinary subject: orthodontics, functional orthopedic, pediatric dentistry, ENT, pediatric and speech therapy. So much so that various areas of medicine have studied possible craniofacial changes in children with respiratory obstruction11-15. The absence of a direct relationship between the cause of airway obstruction and its effect on craniofacial growth11-15 leads to a considerable controversy in the literature. The most accepted theory is that tonsil hyperplasia leads to pharyngeal obstruction, causing mouth breathing, and changes to the position of orofacial and mandible muscles11. These changes, in turn, influence chewing, swallowing and speech, and lead to occlusal and skeletal changes.19-21 The results of this study show that in the group of atypical swallowing, there is airway reduction. Perhaps, such reduction is caused by hyperplasia of the palatine tonsil, leading to pharyngeal obstruction, causing mouth breathing. Data from this study may corroborate the hypothesis of the relationship between mouth breathing and atypical swallowing21. We suggest further studies to evaluate this hypothesis.
Authors have suggested oral breathing as an etiologic factor in atypical swallowing18, 19.21. The results from this study do not enable us to answer to this hypothesis. However, we believe that reducing the oropharyngeal space, as assessed by PAS in this study, is the main cause of both: mouth breathing and atypical swallowing. We believe that atypical deglutition and mouth breathing should be evaluated and treated together. We also believe that these disorders are part of a more complex picture, in which atypical swallowing and mouth breathing are just part of the problem.
CONCLUSIONS- The cephalometric analysis of the PAS revealed a mean difference of about 3 mm between the two groups, with statistical significance;
- The PAS distance, based on radiographic measurements, was lower in children with atypical swallowing.
ACKNOWLEDGEMENTSWe thank CAPES for the financial support.
REFERENCES1. Peng CL, Jost-Brinkmann PG, Yoshida N, Miethke RR, Lin CT. Differential diagnosis between infantile and mature swallowing with ultrasonography. Eur J Orthod. 2003;25(5):451-6.
2. Graber TM, Rakosi T, Petrovic AG. Dentofacial orthopedics with functional appliances. St. Louis: C. V. Mosby Company; 1985. p.139-60.
3. Peng CL, Jost-Brinkmann PG, Yoshida N, Chou HH, Lin CT. Comparison of tongue functions between mature and tongue-thrust swallowing--an ultrasound investigation. Am J Orthod Dentofacial Orthop. 2004;125(5):562-70.
4. Ovsenik M, Farcnik FM, Korpar M, Verdenik I. Follow-up study of functional and morphological malocclusion trait changes from 3 to 12 years of age. Eur J Orthod. 2007;29(5):523-9.
5. Bertolini MM, Vilhegas S, Norato DY, Paschoal JR. Cephalometric evaluation in children presenting adapted swallowing during mixed dentition. Int J Orofacial Myology. 2003;29:29-41.
6. Cayley AS, Tindall AP, Sampson WJ, Butcher AR. Electropalatographic and cephalometric assessment of myofunctional therapy in open-bite subjects. Aust Orthod J. 2000;16(1):23-33.
7. Cheng CF, Peng CL, Chiou HY, Tsai CY. Dentofacial morphology and tongue function during swallowing. Am J Orthod Dentofacial Orthop. 2002;122(5):491-9.
8. Machado Júnior AJ, Crespo AN. Radiographic position of the hyoid bone in children with atypical deglutition. Eur J Orthod. 2012;34(1):83-7.
9. de Felício CM, Folha GA, Ferreira CL, Medeiros AP. Expanded protocol of orofacial my functional evaluation with scores: Validity and reliability. Int J Pediatr Otorhinolaryngol. 2010;74(11):1230-9.
10. Ceylan I, Oktay H. A study on the pharyngeal size in different skeletal patterns. Am J Orthod Dentofac Orthop. 1995.108(1):69-75.
11. Valera FC, Travitzki LV, Mattar SE, Matsumoto MA, Elias AM, Anselmo-Lima WT. Muscular, functional and orthodontic changes in preschool children with enlarged adenoids and tonsils. Int J Pediat Otorhinolaryngol. 2003;67(7):761-70.
12. Valera FC, Trawitzki LV, Anselmo-Lima WT. Myofunctional evaluation after surgery for tonsils hypertrophy and its correlation to breathing pattern: a 2-year-follow up. Int J Pediat Otorhinolaryngol. 2006;70(2):221-5.
13. Paskay L. Instrumentation and measurement procedures in orofacial myology. Int J Orofacial Myology. 2006;32:37-57.
14. Adamidis IP, Spyropoulos MN. The effects of lymphadenoid hypertrophy on the position of the tongue, the mandible and the hyoid bone. Eur J Orthod. 1983;5(4):287-94.
15. Cheng MC, Enlow DH, Papsidero M, Broadbent BH Jr, Oyen O, Sabat M. Developmental effects of impaired breathing in the face of the growing child. Angle Orthod. 1988;58(4):309-20.
16. Malkoc S, Usumez S, Nur M, Donaghy CE. Reproducibility of airway dimensions and tongue and hyoid positions on lateral cephalograms. Am J Orthod Dentofacial Orthop. 2005;128(4):513-6.
17. Rocabado M. Biomechanical relationship of the cranial, cervical and hyoid regions. J Craniomandibular Pract. 1983;1(3):61-6.
18. Machado Júnior AJ, Crespo AN. A lateral cephalometric x-ray study of selected vertical dimensions in children with atypical deglutition. Int J Orofacial Myology. 2010;36:17-26.
19. Kikyo T, Saito M, Ishikawa M. A study comparing ultrasound images of tongue movements between open bite children and normal children in the early mixed dentition period. J Med Dental Sci. 1999;46(3):127-37.
20. Kawashima S, Peltomäki T, Sakata H, Mori K, Happonen RP, Rönning O. Craniofacial morphology in preschool children with sleep-related breathing disorder and hypertrophy of tonsils. Acta Paediatr. 2002;91(1):71-7.
21. Lemos CM, Junqueira PAS, Gómez MVSG, Faria MEJ, Basso SC. Study of the relationship between the dentition and the swallowing of mouth breathers. Intl Arch Otorhinolaryngol 2006;10(2):114-8.
22. Vieira MD, Vilella OV. Cephalometric evaluation of the oropharyngeal space in cases of atypical swallowing. Rev Odonto Ciênc. 2008;23(1):26-30.
23. Salles C, Campos PSF, Andrade NA, Daltro C. Obstructive sleep apnea and hypopnea syndrome: cephalometric analysis. Braz J Othorinolayngol. 2005;71(3):369-72.
1. DDS, Specialist in maxillary functional orthopedics; MSc in Medical Sciences - Unicamp (PhD student - School of Medical Sciences - University of Campinas - Unicamp).
2. PhD (Head of the ENT program - Unicamp).
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on July 21, 2011.
Accepted on September 25, 2011. Code. 8692.
CAPES.
FMC - Unicamp.


