INTRODUCTIONVocal fold immobility is the term that describes restricted movement of vocal folds secondary to mechanical fixation or neurological involvement. Mobility of the vocal folds may be decreased or absent, and it may be unilateral or bilateral. From the standpoint of the etiology, choice of treatment, and prognosis, it is important to differentiate between hypomobility and immobility, as well as unilateral or bilateral involvement1.
There are two forms by which patients may present bilateral vocal fold immobility: existing stridor for weeks or months that worsens rapidly to dyspnea or progressive and gradual dyspnea in the course of a few months2, usually with no significant changes in voice quality.
The diagnosis and treatment of bilateral vocal fold immobility has been studied often in laryngology during the past few decades; several studies have described approaches that rehabilitate the larynx with a high success rate3.
Bilateral vocal fold immobility is a potentially fatal condition; it needs to be diagnosed promptly and accurately, and treated appropriately2. Bilateral vocal fold immobility may be caused by bilateral neurogenic palsy, fixation of the cricoarythenoid joint, laryngeal synechiae, or posterior glottic stenosis2. The differential diagnosis is based on the medical history, fibronasopharyngolaryngoscope findings, and laryngeal electromyography. In a few cases, the diagnosis is only possible by inspecting and palpating the larynx by microlaryngoscopy. Specific causes may be surgical trauma, post-intubation trauma, cancer, neurologic conditions, inflammatory diseases, and psychogenic causes4.
The treatment of bilateral vocal fold immobility aims to reestablish a patent airway, to preserve glottic sphincter function, and to maintain voice quality5. Existing surgical options are tracheotomy, total arythenoidectomy, subtotal arythenoidectomy, transverse cordectomy, vocal fold lateralization6, and open and reinnervation techniques7.
OBJECTIVEThe purpose of this study was to analyze the diagnostic methods and therapeutic approaches in cases of bilateral vocal fold immobility seen at our unit.
MATERIALS AND METHODSThe institutional review board assessed and approved this study (protocol no. 114/010. This was a retrospective quantitative study consisting of a review of patient registries diagnosed with bilateral vocal fold immobility by fibronasolaryngoscopy at our unit from 1992 to 2007. The cases were classified according to the etiology: (1) due to neurologic involvement (palsy); and (2) due to a decreased diameter of the posterior glottis (posterior glottic stenosis), in which case it was classified according to Bogdasarian & Olson8 (Table 1).
The etiology was defined based on the clinical history, the physical examination, and diagnostic tests such as electroneuromyography (EMG) and computed tomography (CT), if needed; it was compared with data in the available literature.
The type of treatment was analyzed according to the etiology and the degree and type of upper airway narrowing. Success was defined as a patent airway with preservation of the glottic sphincter function and voice quality.
RESULTSThe sample comprised 35 patients with a diagnosis of bilateral vocal fold immobility at our unit from 1992 to 2007. Of this total, 18 cases (51.4%) presented bilateral vocal fold palsy, and 17 cases (48.6%) had posterior glottic stenosis.
Of the 18 patients with bilateral vocal fold palsy, four were male and 14 were female. The mean age was 45 years, ranging from 18 to 65 years. The etiology of bilateral vocal fold immobility was as follows: after thyroidectomy in 16 patients (88.9%), extrinsic compression of the mediastinum by a rhinopharyngeal lymphoepithelioma with lung metastasis in one patient (5.55%), and recurrence following resection of a mediastinal paraganglioma one patient (5.55%).
Among the patients with bilateral vocal fold palsy, laryngoscopy showed bilateral vocal fold immobility in adduction in 17 cases (94.4%), of which only four had tracheotomies. These patients underwent laryngeal microsurgery under general anesthesia to perform CO
2 laser subtotal unilateral arytenoidectomy (Remacle)9 preserving a small posterior shell-shaped portion of the arytenoid cartilage. Granulation tissues formed in the arytenoid resection bed in two patients, which required surgical reexploration. Transitory aspiration occurred in four patients, and resolved spontaneously. Previously tracheostomized patients were decannulated on average 40 days after surgery. Only the patient with mediastinal paraganglioma had vocal fold immobility in abduction, and underwent type I thyroplasty.
Of 17 patients with posterior glottic stenosis (Table 2), 13 were male and four were female. The mean age was 44.7 years, ranging from 9 to 74 years. The etiology of stenosis was as follows: bilateral vocal fold immobility after prolonged orotracheal intubation in 15 patients (88.2%), after radiotherapy for laryngeal squamous cell carcinoma in one patient (5.9%), and after removal of a large laryngeal papilloma in one patient (5.9%). Posterior glottic stenosis was classified according to Bogdasarian & Olson8 (Table 1). It was type II in 10 cases (58.8%), type III in five cases (29.4%) (Figure 1), and type IV in two cases (11.8%) (Graph 1).
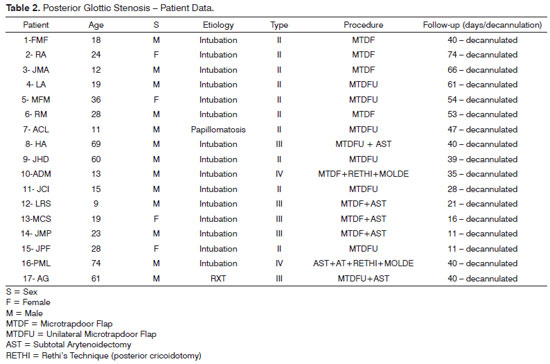
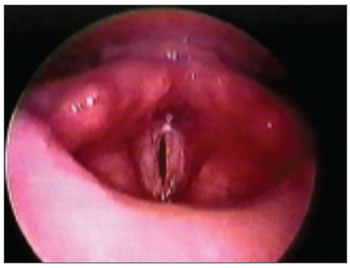
Figure 1. Posterior glottic stenosis grade III.
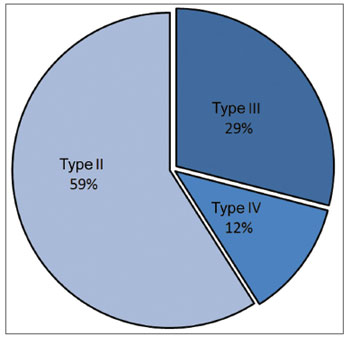
Graph 1. Type of posterior glottic stenosis in the series (Bogdasarian and Olson classification8).
The microtrapdoor flap technique first described by Dedo & Sooy10 was used initially in eight patients (47%) (Figure 2) with posterior glottic stenosis. In this technique, an incision is made on the superior surface of the stenosis, the submucosa is dissected with CO
2 laser to create a bipediculated lateral mucous flap, and the underlying scar tissue is removed. A variant of the microtrapdoor flap was used in eight patients (47%); in these cases, a vertical incision was made on the vocal process on one side and extended through a horizontal incision on the posterior interarytenoid surface to the other side, thereby creating a crescent moon-shaped unilaterally based mucous flap. The submucosal scar is easily vaporized by CO
2 laser (0.25 mm microspot, superpulse mode, 5 watts). The mucous flap is thinned and placed over the open surface on one side and fixed with fibrin gel on the site (Tissucol
®). This is the unilateral microtrapdoor flap technique.

Figure 2. Unilateral microtrapdoor flap: posterior glottic stenosis grade III.
Subtotal arytenoidectomy associated with the microtrapdoor flap was done in five patients (29.4%) with posterior glottic stenosis involving one of the cricothyroid joints, as described by Remacle.9
Decannulation was only possible after laryngofissure, posterior cricoidotomy, removal of scar tissue, placement of a cartilage graft and molding (Rethi's technique)11 in one patient (6%) with severe posterior glottic stenosis (Type IV) that had undergone microtrapdoor flap surgery. Subtotal arytenoidectomy, followed by total arytenoidectomy, as described by Ossoff12,13, was done in a second procedure; the arytenoid cartilage was removed, the muscle and vocal process were removed with laryngofissure and posterior cricoidotomy (Rethi's technique)11, and laryngeal molding was done (and removed 18 days later) in one patient (6%) with type IV posterior glottic stenosis.
The perception of voice in these patients according to the RASAT score was as follows:
- patients undergoing partial arytenoidectomy at first had moderate soprosity that regressed with speech therapy;
- the quality of voice did not worsen in patients undergoing the microtrapdoor flap procedure;
- patients undergoing more extensive procedures (Rethi + molding) had persisting moderate roughness and soprosity.
All patients had acceptable voice communication with mild to moderate degrees of dysphonia.
DISCUSSIONBilateral vocal fold immobility in adduction reduces the volume of the glottic space, and consequently increases airway resistance, which induces persistent dyspnea that worsens with exercise and upper airway inflammatory conditions. An accurate diagnosis and appropriate treatment is needed as this condition may progress to acute respiratory failure.
Bilateral vocal fold immobility may be diagnosed by fibronasopharyngolaryngoscopy, which will show lack of movement of both vocal folds. It may result from palsy of the recurrent laryngeal nerve or from posterior glottic stenosis. These conditions may present similar findings and the clinical history with endoscopy may not always differentiate these diseases. At this moment, laryngeal EMG is indicated for the etiological and differential diagnosis14. The action potential of thyroarytenoid muscles was evaluated by EMG in this study. Paralysis was excluded if the action potential of both thyroarytenoid muscles was unaltered; in these cases, the diagnosis was posterior glottic stenosis. Recurrent laryngeal nerve palsy was diagnosed if the action potential was abnormal.
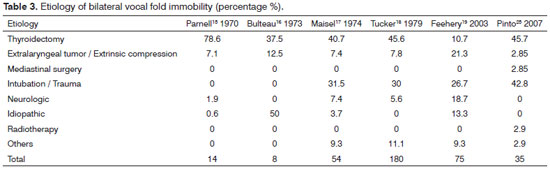
Most studies on the etiology of bilateral vocal fold immobility have suggested that post-thyroidectomy bilateral vocal fold palsy is the most common cause15-18. (Table 3). Feehery19 has shown that few papers have been published on this topic since 1980. His comparative study of the etiologic factors reported before and after 1980 showed a significant increase in cases of bilateral vocal fold immobility due to trauma (non-surgical and post-surgical intubation not due to thyroidectomy) and extrinsic compression by neoplasms (27% post-trauma, 21% due to neoplasms, 11% post-thyroidectomy)19. Rosenthal et al.20 studied the etiology of bilateral vocal fold immobility in the past 20 years also showed a lower incidence of bilateral palsy by iatrogenic causes in surgery. In our study, 16 of 35 patients (45.7%) had post-thyroidectomy bilateral vocal fold immobility, and 15 patients (42.8%) had this condition after prolonged intubation, which is comparable to recent papers on this topic.
Several surgical procedures have been proposed for the treatment of bilateral vocal fold immobility due to bilateral vocal fold palsy; these include external and endoscopic procedures21-25. Endoscopic approaches started with arytenoidectomy by electrocautery (Thornell)26 and CO
2 laser total arytenoidectomy (Ossoff)12. Another conservative technique25-29 is subtotal arytenoidectomy (Remacle)9.
All of the patients in our sample with bilateral vocal fold immobility due to bilateral vocal fold palsy in adduction underwent subtotal arytenoidectomy (Remacle's technique)9. The success rate was 100% - all patients had patent airways. There were no post-operative complications except for transitory aspiration that resolved spontaneously, and a granuloma in one patient that was excised surgically.
Treatment of posterior glottic stenosis is still difficult; there are several available procedures and techniques, including endoscopic dilatation30, corticosteroids injected into lesions8, laryngofissure with posterior cricoidotomy11, excision of scars with placement of skin or mucosal grafts, and placement of different types of molds10,31,32.
We initially used the microtrapdoor flap technique bilaterally, according to Dedo & Sooy's10 original technique, in eight patients with a larger amount of interarytenoid mucous tissue. Subtotal arytenoidectomy was also done in five of these patients because of unilateral cricoarytenoid joint anquilosis. In two patients with severe posterior glottic stenosis (type IV) - one of which had been operated with the microtrapdoor flap technique and the other with subtotal arytenoidectomy - deccanulation was only possible after laryngofissure and posterior cricoidotomy with resection of scar tissue, graft placement, and molding (Rethi's technique11).
The unilateral microtrapdoor flap technique was used in another eight cases of posterior glottic stenosis, as the incision facilitates dissection and better exposure of the stenotic scar. This technique was effective in 100% of cases; it was associated with subtotal arytenoidectomy in two of the type III posterior glottic stenosis cases (Figure 3).

Figure 3. Post-operation - unilateral microtrapdoor flap.
An ideal treatment of bilateral vocal fold immobility has not been found in spite of advances in surgery and laryngology materials. Current techniques restore airway patency at the cost of possible worse sphincter function and voice quality. Research on laryngeal reinnervation has yielded improved muscle tone, less atrophy and vocal fold bowing, but no mobility gains33. Another promising line of research is of implantable stimulators, which maintain mobility and voice patterns, but as yet have yielded results only in experimental studies34.
Because this was a retrospective study, it is difficult to make accurate short/long term quantitative and qualitative analyses. However, the results are similar to those in the literature; further studies are needed to carefully evaluate these data.
CONCLUSIONBilateral vocal fold immobility is a potentially fatal condition; for this reason, accurate and prompt diagnosis followed by adequate treatment is mandatory. It is essential to differentiate palsy from vocal fold fixation in cases of bilateral vocal fold immobility so that the treatment is selected accordingly. EMG is indicated for this purpose.
Subtotal arytenoidectomy with a microscope is our choice of surgery for the treatment of bilateral vocal fold palsy in adduction. The choice of surgery in posterior glottic stenosis cases depends on the degree of stenosis (microtrapdoor flap and unilateral microtrapdoor flap in isolation or associated with subtotal arytenoidectomy and/or laryngofissure with posterior cricoidotomy - Rethi's technique).
REFERENCES1. Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007;117(10):1864-70.
2. Krishna P, Rosen CA. Office-based arytenoid palpation for diagnosis of disorders of bilateral vocal fold immobility. Ear Nose Throat J. 2006;85(8):520-2.
3. Merati AL, Shemirani N, Smith TL, Toohill RJ. Changing trends in the nature of vocal fold motion impairment. Am J Otolaryngol. 2006;27(2):106-8.
4. Hillel AD, Benninger M, Blitzer A, Crumley E, Flint P, Kashima HK, et al. Evaluation and management of bilateral vocal fold immobility. Otolaryngol Head and Neck Surg. 1999;121(6):760-5.
5. Motta S, Moscillo L, Imperiali M, Motta G. CO2 laser treatment of bilateral vocal cord paralysis in adduction. ORL J Otorhinolaryngol Relat Spec. 2003;65(6):359-65.
6. Bosley B, Rosen CA, Simpson CB, McMullin BT, Gartner-Schmidt JL. Medial arytenoidectomy versus transverse cordotomy as a treatment for bilateral vocal fold paralysis. Ann Otol Rhinol Laryngol. 2005;114(12):922-6.
7. Tucker HM. Long-term results of nerve-pedicle reinnervation for laryngeal paralysis. Ann Otol Rhinol Laryngol. 1989;98(9):674-6.
8. Bogdasarian RS, Olson NR. Posterior glottic laryngeal stenosis. Otolaryngol Head Neck Surg. 1980;88(6):765-72.
9. Remacle M, Lawson G, Mayné A, Jamart J. Subtotal carbon dioxide laser arytenoidectomy by endoscopic approach for treatment of bilateral cord immobility in adduction. Ann Otol Rhinol Laryngol. 1996;105(6):438-45.
10. Dedo HH, Sooy CD. Endoscopic laser repair of posterior glottic, subglottic and tracheal stenosis by division or micro-trapdoor flap. Laryngoscope. 1984;94(4):445-50.
11. Rethi A. An operation for cicatricial stenosis of the larynx. J Laryngol Otol. 1956;70(5):283-93.
12. Ossoff RH, Sisson GA, Duncavage JA, Moselle HI, Andrews PE, McMillan WG. Endoscopic laser arytenoidectomy for the treatment of bilateral vocal cord paralysis. Laryngoscope. 1994;94(10):1293-7.
13. Ossoff RH, Duncavage JA, Shapshay SM, Krespi YP, Sisson GA Sr. Endoscopic laser arytenoidectomy revisited. Ann Otol Rhinol Laryngol. 1990;99(10 Pt 1):764-71.
14. Simpson DM, Sternman D, Graves-Wright J, Sanders I. Vocal cord paralysis: clinical and eletrophysiologic features. Muscle Nerve. 1993;16(9):952-7.
15. Parnell FW, Brandenburg JH. Vocal cord paralysis. A review of 100 cases. Laryngoscope. 1970;80(7):1036-45.
16. Bulteau V. The aetiology of bilateral recurrent laryngeal nerve paralysis. Med J Aust. 1973;2(16):776-7.
17. Maisel RH, Ogura JH. Evaluation and treatment of vocal fold paralysis: a review of 100 cases. Laryngoscope. 1974;84:302-16.
18. Tucker HM. Vocal cord paralysis-1979: etiology and management. Laryngoscope. 1980;90(4):585-90.
19. Feehery JM, Pribitkin EA, Heffelfinger RN, Lacombe VG, Lee D, Lowry LD, et al. The evolving etiology of bilateral vocal fold immobility. J Voice. 2003;17(1):76-81.
20. Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007;117(10):1864-70.
21. Jackson C. Ventriculocordectomy, a new operation for the cure of glottic stenosis. Arch Surg. 1922;4:257-74.
22. Hoover WB. Bilateral abductor paralysis, operative treatment of submucous resection of the vocal cord. Arch Otolaryngol. 1932;15:337-55.
23. King BT. A new and function restoring operation for bilateral abductor cord paralysis. JAMA. 1939;112:814-23.
24. Woodman D. A modification of the extralaryngeal approach to arytenoidectomy for bilateral abductor paralysis. Arch Otolaryngol. 1946;43(1):63-5.
25. Pinto, JA. Cirurgia das paralisias bilaterais da laringe. Tratado de Otorrinolaringologia, vol V, pag 422-426, liv. Roca, São Paulo, 2003.
26. Thornell WC. Intralaryngeal approach for arytenoidectomy in bilateral abductor vocal cord paralysis. Arch Otolaryngol. 1948;47:505-8.
27. Crumley RL. Endoscopic laser medial arytenoidectomy for airway management in bilateral laryngeal paralysis. Ann Otol Rhinol Laryngol. 1993;102(2):81-4.
28. Dennis DP, Kashima H. Carbon dioxide laser posterior cordectomy for treatment of bilateral vocal cord paralysis. Ann Otol Rhinol Laryngol. 1989;98(12 Pt 1):930-4.
29. Kashima HK. Bilateral vocal fold motion impairment: pathophysiology and management by transverse cordotomy. Ann Otol Rhinol Laryngol. 1991;100(9 Pt 1):717-21.
30. Benjamin B. Endolaryngeal Surgery. 1st ed, United Kingdom: Martin Dunitz; 1998.143-68.
31. Montgomery WW. Posterior and complete laryngeal stenosis. Arch Otolaryngol. 1973;98(3):170-5.
32. Langman AW, Lee KC, Dedo HH. The endoscopic Teflon keel for posterior and total glottic stenosis. Laryngoscope. 1989;99(6 Pt 1):571-7.
33. Aynehchi BB, McCoul ED, Sundaram K. Systematic review of laryngeal reinnervation techniques. Otolaryngol Head Neck Surg. 2010;143(6):749-59.
34. Nomura K, Kunibe I, Katada A, Wright CT, Huang S, Choksi Y, Mainthia R, Billante C, Harabuchi Y, Zealear DL. Bilateral motion restored to the paralyzed canine larynx with implantable stimulator. Laryngoscope. 2010;120(12):2399-409.
1. Otorhinolaryngologist. Director/Head.
2. Medical doctor, otorhinolaryngologist, assistant physician at the São Paulo Otorhinolaryngology and Head & Neck Surgery Unit.
3. Medical doctor, otorhinolaryngologist, assistant physician at the São Paulo Otorhinolaryngology and Head & Neck Surgery Unit.
4. Medical resident of the São Paulo Otorhinolaryngology and Head & Neck Surgery Unit.
5. Medical resident of the São Paulo Otorhinolaryngology and Head & Neck Surgery Unit.
São Camilo Hospital and Maternity - Pompeia (Hospital e Maternidade São Camilo - Pompéia).
Send correspondence to:
Jose Antonio Pinto
Alameda dos Nhambiquaras, 159
São Paulo - SP. CEP: 04090-010
Phone. (0xx11) 5573-1970
E-mail: japorl@uol.com.br
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on October 22, 2010
Accepted on February 6, 2011. cod. 7384
São Paulo Otorhinolaryngology and Head & Neck Surgery Unit (Núcleo de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço de São Paulo).


