INTRODUCTIONA probe microphone measurement is an objective and accurate technique to check whether hearing aid (HA) performance in the user's ear fits into a certain curve or set or curves (gain or output per prescribed frequency); it is considered best practice for hearing aid fitting1-7. There are reports stating that about 23%-40% of professionals routinely use such measurements in clinical practice8-10.
Use of digital HAs has been accompanied by a growing trust by professionals in programming software simulations and calculations, rather than empirical verification of HA fit11.
Such software have become more sophisticated and at the same time user friendly, providing clinicians with interactive programming procedures, electronic fine tuning guides, and several visualization options as to how a given HA is being programmed - such as simulated gain curves and output1,12. However, even if software demonstrates an equivalence between HAs and prescriptions, these simulations do not truly reflect the performance of these devices in the user's ear. Studies have shown that software simulations tend to overestimate the amplification that is actually provided to the real ear12-14.
The purpose of this study was to compare HA software programming simulated insertion gain with true insertion gain measurements.
METHODThe institutional review board approved this study (no. 28/2009).
A retrospective study was made of the registries of patients seen from January to July 2009; enrolment was done according to the following criteria:
- age group: adults (aged over 18 years),
- no outer or middle ear alterations as seen in the otorhinolaryngological examination,
- sensorineural hearing loss of varied degrees,
- users of software programmable HA with the NOAH 3.0 application,
- programming software with a simulated insertion gain option using the same parameters as those used in real ear measurements (speech spectrum stimulus, and presentation level at 65 dB SPL),
- HA evaluated with the noise reduction algorithm turned off.
Data was gathered from the registries of 62 patients (30 male and 32 female) aged from 29 to 93 years (mean - 71 years) with mild to severe unilateral (n=14) or bilateral (n=48) sensorineural hearing loss. The total number of ears was 110.
Table 1 shows the number of patients according to age groups (10-year intervals).
Probe microphone measurements were done in acoustic booths that were large enough for patients to be seated one meter away from the loudspeaker at 0˚ azimuth. The examiner used the geometric method to position the probe tube for in situ measurements. Thus, the probe tube was aligned along the medial ear mold position and measured so that it remained 5.0 mm beyond the tip of the patient's ear mold and 5.0 to 6.0 mm from the tympanic membrane. A marker ring was placed on the intertragic notch to check the probe tube length to be inserted in the outer ear canal of the patient. A speech noise signal at 65 dB SPL was used for the measurements. An Aurical (Madsen) device was used for results analysis.
The database of the NOAH 3.0 platform was used to gather data on software programming simulated insertion gain from two HA providing companies, which presented simulation data as simulated insertion gain charts per frequency generated by a speech noise stimulus at 65 dB.
The software simulation results and real ear measurements at 250 to 4000 Hz interoctave bands were recovered and annotated in a specific protocol.
The statistical analysis was made with the
Pacote Estatístico (PACOTICO) software. The paired t test was applied to compare the true insertion gain with the simulated insertion gain at each test frequency. Pearson's correlation coefficient was applied to check for correlations between age and the difference between software simulated and real ear values. The significance level (α) was = 0.05 in all cases.
RESULTSFigure 1 presents the true and simulated gains per frequency and their significance.
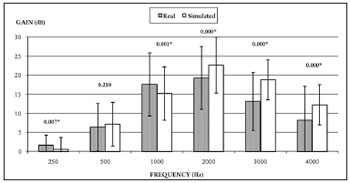
Figure 1. Comparison between true gain obtained from measurements with a microfone sonda and simulated gain in the hearing aid programming software at 250-4000 Hz (n=110).
Table 2 shows the correlations among age and differences between simulated and true gains and their significance.
DISCUSSIONFigure 1 shows that there was a significant difference between simulated and real insertion gains at all frequencies except 500 Hz; such differences were larger at higher frequencies.
Differences between true and simulated gains have been noted in the literature12. A study of 12 patients showed that differences between true and simulated gains were 0 dB (± 5 dB standard deviation) from 250 to 1000 Hz. However, at higher frequencies, more patients showed substantial decreases in true insertion gains compared to simulated gains. Furthermore, negative difference values for most patients indicated that simulated insertion gains overestimated the true insertion gains in real ears. Such data agree with the findings of the present study, where the largest differences were encountered at 2000 to 4000 Hz. The values of real ear insertion gains were higher compared to simulated insertion gains at 250 to 1000 Hz; we found no reports of such inversion of differences in the literature.
A few authors13 have stated that real ear measurements simulated in HA programming software are not accurate, and tend to overestimate individually obtained values. These values were 0.5 dB lower at 1000 Hz and over 4000 Hz. True insertion gain values are closer to simulated insertion gain values at frequencies from 1500 to 4000 Hz. Our data revealed differences even at frequencies from 2000 to 4000 Hz; we were unable to assess frequencies over 4000 Hz because of limitations in the software charts of companies supplying HAs.
Results have shown that 64% of fits did not reach the prescribed insertion gain by the NAL-NL1 rule at one or more frequencies from 250 to 4000 Hz when the first fit or quick set option was chosen in the programming software14.
Correlations between age and simulated and true gain were weak and not significant (Table 2). We assume these results are due to a homogeneous study sample, since most subjects were aged from 70 to 90 years (Table 1).
Thus the importance of including probe microphone measurements according to current protocols in the verification process, making HA fitting a more objective process based on scientific evidence. Programming software are essential tools that provide interactivity with technology and enable more accurate adjustments. However, it is important to evaluate the meaning of each simulation chart and to interpret them as a starting point in HA fitting - a preadjustment with posterior verification should be considered.
Professionals should learn how companies providing these devices have generated the simulation values, which may be used as a first step.
CONCLUSIONThis study enabled us to assess differences between simulated and true (real ear) insertion gain values.
No correlation was found between age of participants and the differences between simulated and true insertion gain values; there were, however, a difference between true and simulated gain.
REFERENCES1. Dillon H, Keidser G. Is probe-mic measurement of HA gain-frequency response best practice? The Hearing Journal [serial on the internet]. 2003 [cited 2009 Nov 09]; 56(10):28-30. Available from: http://www.audiologyonline.com/theHearingJournal/pdfs/HJ2003_10_pg28-30.pdf.
2. Valente M, Abrams H, Benson D, Chisolm T, Citron D, Hampton D, et al. Guidelines for the audiological management of adult hearing impairment. Audiology Today [serial on the internet]. 2006 [cited 2009 Dec 09];18(5). Available from: http://www.audiology.org/resources/documentlibrary/Documents/haguidelines.pdf.
3. American Academy of Audiology. Guidelines for the audiologic management of adult hearing impairment. United States: AAA, 2008.
4. Mueller GH. Probe-mic measurements: Hearing aid fitting's most neglected element. Hearing Journal [serial on the internet]. 2005[cited 2009 Dec 09]; 58(10):21-30. Available from: http://www.audiologyonline.com/theHearingJournal/pdfs/HJ2005_10_pg21-30.pdf
5. Yanz JL, Pisa JFD, Olson L. Integrated REM: real-ear measurement from a hearing aid. Hearing Review. [serial on the internet]. 2007 [cited 2009 dec 09]. Available from: http://www.hearingreview.com/issues/articles/2007-05_04.asp.
6. Frye GJ. El examen del audıfono digital. Auditio: Revista electronica de audiologıa. [serial on the internet]. 2002 [cited 2009 Nov 09]; 1(2):25-9. Available from: http://www.auditio.com/revista/pdf/vol1/2/010203.pdf.
7. Kuk FK. Considerations in modern multichannel nonlinear hearing aids. In: Valente M. Hearing aids: standards, options, and limitations. 2
nd. New York: Thieme, 2002. p. 178-213.
8. Muller GH. Fitting hearing aids to adults using prescriptive methods: an evidence-based review of effectiveness. J Am Acad Audiol [serial on the internet]. 2005 [cited 2009 July 12]; 16(7):448-60. Available from: http://docserver.ingentaconnect.com.w10077.dotlib.com.br/deliver/connect/aaa/10500545/v16n7/s5.pdf?expires=1247436740&id=51166152&titleid=72010016&accname=Universidade+de+Sao+Paulo+%28USP%29&checksum=D182D3EE89ADC71ED37D26E5C932C6BB.
9. Kirkwood D. Survey: Dispensers fitted more hearing aids in 2005 at higher prices. Hear J. 2006;59(4):48.
10. Strom KE. The HR 2006 dispenser survey. Hearing Review. 2006;13(6):34
11. Fabry DA. Nonlinear Hearing Aids and Verification of Fitting Targets. Trends Amplif. 2003;7(3):99-115
12. Hawkins DB, Cook JA. Hearing aid software predictive gain values: How accurate are they? The Hearing Journal [serial on the internet]. 2003 [cited 2009 Nov 09]; 56(7):26-34. Available from: http://www.audiologyonline.com/theHearingJournal/pdfs/HJ2003_07_pg26-34.pdf.
13. Aarts NL, Caffee CS. Manufacturer predicted and measured REAR values in adult hearing aid fitting: accuracy and clinical usefulness. Int J Audiol. 2005;44(5):293-301.
14. Aazh H, Moore BCJ. The value of routine real ear measurement of the gain of digital hearing aids. J Am Acad Audiol [serial on the internet]. 2007 [cited 2009 Dec 07]; 18(8):653-64. Available from: http://docserver.ingentaconnect.com.w10077.dotlib.com.br/deliver/connect/aaa/10500545/v18n8/s3.pdf?expires=1260198091&id=53835920&titleid=72010016&accname=Universidade+de+Sao+Paulo+%28USP%29&checksum=25E4708B8CDE39B58EDDB34DD5BB3BE8.
1. Specialist in clinical and educational audiology, Federal Board of Speech Therapy. Laboratory specialist on hearing aids, Speech Therapy Department, Bauru Dentistry School, São Paulo University.
2. Doctoral degree in communication disorders, HRAC, São Paulo University. Assistant professor of the speech therapy course, Bauru Dentistry School, São Paulo University.
3. Doctoral degree in neuroscience and neuropsychology, São Paulo University. Assistant professor of the speech therapy course, Bauru Dentistry School, São Paulo University.
Bauru Dentistry School, São Paulo University.
Send correspondence to:
Maria Fernanda Capoani Garcia Mondelli
R. Ivane de Andrade Almeida, 1-55, Cond. Villaggio I
Bauru - SP. CEP: 17018-825
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on May 28, 2010
Accepted on July 23, 2010. cod. 7127


