IntroductionThe term mucoceles was introduced by Rollet (1896) and characterizes the expansive benign cystic lesion of the epithelium lining resulting in mucus accumulation in the obstructed cavity. 1.
Mucoceles is characterized by slow evolution along many years, unless it has complications such as infection. If the mucoceles does become infected it is known as mucopyocele.7
It is a relatively uncommon condition and frequently occurs in the fronto-ethmoidal region probably due to the complex draining system of these sinuses, followed by maxillary and sphenoid regions.4 It affects both male and female with no preference for gender, mostly aged from 30 to 40 years, but it may also affect children.2
The obstructive factor in the drainage area of the sinus is viewed as the cause of this cavity obstruction. The etiology can be divided in obstructive strictly speaking: polyps, trauma, surgery and tumor compression, and inflammatory: infection, cystic degeneration, increased mucous secretion and allergy cause.7
Its causes can be primary or secondary. Primary causes would originate from a mucous gland of the submucosa, however, it is not well accepted since some facts such as few mucosa glands in the frontal sinus and histological studies did not show evidence of preexisting retention as the origin of mucoceles. Secondary cause, in which mucoceles is viewed as a consequence of sinus drainage obstruction, has sustained itself as the major cause of this disease.8
Mucoceles will cause symptoms if sinuses margin suffer erosion (mainly in the superior-medial margin of the orbit), causing skin bulging or eyeball alterations. 3 Frequently, fronto-ethmoidal mucoceles cause ocular proptosis, and it still may expand to nasal fossa and anterior cranial fossa.
Radiography and sonography may be used for diagnosis, however final diagnosis will be provided by CT and MRI. 9
Management consists basically of surgery to clear the cavity and to reestablish communication with nasal fossa.
Material and Methods Thirteen (13) patients diagnosed with fronto-ethmoidal mucoceles by endoscopy endonasal approach were treated in the Rhinology center of the Otorhinolaryngology Department of EPM from January 2000 through April 2001. Endoscopic surgery equipment was rigid 4mm Hopkins Machida endoscope (0 and 30 degrees) and a Storz (45 degrees). Surgeries were conducted under general anesthesia and topical adrenaline solution at 1:1000 for vasoconstriction. Palpation of the lesion with the Freer elevator or aspirator and the clearance of mucoceles were conducted by aspirating the secretion inside it and the material was sent to be analyzed in laboratory. After opening the mucoceles, sharp-angled forceps were used to ensure large marsupialization. A rigid Hopkins Machida (30 degrees) endoscope was used postoperatively to inspect and clean the cavity. Postoperative visits occurred in the seventh day, and every two weeks in the first month after the procedure, and then on a monthly basis until the cavity healing had a good aspect.
ResultsThirteen patients underwent surgery (09 male and 04 female) aged from 13 to 68 years (mean of 41.3 years). Seven (07) patients with right side mucoceles and six (06) patients with pathology in the left side. Four (04) patients had the obstructive form as major cause of the condition, one (01) case was due to tumor, and three (03) cases due to trauma, the remaining nine (09) patients had inflammatory form (Table 01).
Table 1.
All patients had old clinical history together with fronto-ethmoidal mucoceles diagnosis, and the major symptoms were diplopia and unilateral proptosis. Two patients had ophthalmologic complications, orbital abscess with ocular fixation and low visual acuity (only luminous perception) and a subperiosteal abscess, with decreased ocular movement and low visual acuity that required orbital decompression in both cases during the surgical procedure. All patients underwent CT at coronal and axial sections during the preoperative period in compliance with the protocol of the Institution; one patient was subjected to MRI for differential diagnosis of CNS pathology. Patients left the surgery with no nasal packing, and no complications were reported. The two patients that underwent orbital decompression had their infection treated with Ciprofloxacin, Clindamycin and Betamethasone during hospital stay, and quinolones for three weeks after discharge. One of the patients improved visual acuity and the other only sustained luminous perception. Patients follow up is still underway on a regular basis with endoscope examinations. No cases of recurrence have been reported up to this moment.
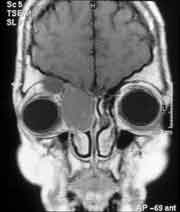
Figura 1.

Figura 2.

Figura 3.

Figura 4.

Figura 5.

Figura 6.

Figura 7.

Figura 8.
The etiology factors are commonly mentioned in the literature and can be divided into those related to anterior recess obstruction and those associated with inflammation. The histological examination of mucoceles mucosa shows chronic inflammation, fibrosis and dynamic balance between mucoceles and bone interface, where osteoclastic and osteoblastic activity result in osteolysis, bone neoformation and sclerosis10.
According to some publications about histological aspects of fronto-ethmoidal mucoceles, the epithelium lining would be changed, with the pseudostratified epithelium progressively expanding to low or cuboid columnar with occasional globlet cells, caused by the erosive pressure of the obstruction. 5 A new theory that evolved in 1991 stated that in addition to the obstruction, the infection with chronic inflammation would have a role in mucoceles through lymphocytes and monocytes that stimulated by the infection would increase prostaglandin and colagenesis in the fibroblasts and the mucous epithelium, which consequently would stimulate bone reabsorption and mucoceles expansion.5
Diagnosis was carried out according to clinical history of long term and wide range of symptoms, which included primarily ophthalmologic symptoms, and the most relevant were ocular proptosis, diplopia that could lower visual acuity if happened simultaneously with infection, as was the case of 02 patients in this study. Imaging examinations are a very useful tool for additional diagnosis and CT cannot be excluded. CT helps in early diagnosis and enables the visualization of the lesion extension and presence of complications, mainly involvement of CNS and orbital cavity. MRI differentiates cerebral tissue and orbital structures from nasal lesion.
Therapy is basically surgery to clear the cavity and to reestablish the communication with nasal fossa. Recently, it has been observed a trend for endoscopic surgery. It replaces the external surgery route used little time ago, in which fronto-ethmoidal mucoceles was approached with Lynch-Howarth incision or osteopathic flap; whereas Cadwell-Luc procedure was reserved to rare cases of maxillary mucoceles. The endoscope access provides a number of advantages, decreased hospital stay and the technique prevents potential complications of external access. Nevertheless, not all fronto-ethmoidal mucoceles are able to be managed purely by endoscope approach; in some cases, such as previous surgery, significant nasosinusal pathology, presence of cutaneous fistula and significant osteomyelitis, the use of combined technique is required.7
The endoscopic surgery is currently considered the treatment of choice of mucoceles in paranasal sinuses, however, depending on the surgeon expertise and presence of complications, endoscope procedure alone cannot be used, and the combined procedure in such cases provides excellent long-term outcome.6
Patients are followed up from 7 to 10 days in the postoperative period and with week visits to ensure success of surgery and to assess satisfactory healing of the cavity. 6
ConclusionEarly diagnosis, support of imaging methods, otorhinolaryngology surgeons' total command of the technique, and single endoscope access result in morbidity decrease in the treatment of mucoceles, which is essentially surgical.
References1. CANALIS,J.G.; ZAJTCHUK,J.T.; JENKINS,H.A. - Ethmoidal Mucoceles. Arch. Otolaryngol., 1978; 104: 268- 91.
2. DIAZ,F.; LATCHOW,R.; DUVALL,A.B. Mucoceles with intracranial and extracranial extensions: Report of two cases. J. Neurosurg., 1978; 48: 248-8.
3. GRANATO,L; LESSA,R.M; RIOS,OAB;MARINHO,V- Mucocele e piocele dos seios paranasais e concha média. Relato de três casos. Rev.Bras.ORL., 2001; 67(1):101-6.
4. KENNEDY,D.W.; JOSEPHONSON,,J.S.; ZINREICH,S.J.; MATTOX, D.E.; GOLDSMITH,M.M.- Endoscopic sinus surgery for mucoceles: A viable alternative. Laryngoscope, 1989; 99: 885 -95.
5. KRISHNAN,G.; KUNAR,G.- Fronto ethmoid mucoceli: one year follow-up endoscopic fronto ethmoidectomy. J. Otolaryngol., 1996; 25(1): 37-40.
6. LUND,V.J.- Anatomical considerations in the etiology of fronto-ethmoidal mucoceles. Rhinology, 1987; 25: 83-8.
7. LUND,V.J.- Endoscopic Management of paranasal sinus mucoceles. J. Laryngol. Otol., 1998; 112: 36-40.
8. LUND,V.J.; MILROY,C.M.- fronto-ethmoidal mucoceles: a histopathological analysis. J. Laryngol. Otol., 1991; 105: 921-3.
9. NATVIG,V.J.; LARSEN,T.E.- Mucoceles of paranasal sinuses. J. Laryngol. Otol., 1978; 92: 982-1075.
10. STIERNBERG,C.M.; BAILEY,B.J.; CALHOUN.K.H.- Management of invasive fronto-ethmoidal sinus mucoceles. Arch. Otolaryngol., 1986; 112 (10): 1060-3.
[1]Master in Otorhinolaryngology, Unifesp-EPM.
[2]Resident Physician, Department of Otorhinolaryngology, Unifesp-EPM.
[3] Resident Physician, Department of Otorhinolaryngology, Unifesp-EPM.
[4]Master studies under course, Department of Otorhinolaryngology, Unifesp-EPM.
Professor, Department of Otorhinolaryngology , Unifesp-EPM, Head of Rhinology, Discipline of Otorhinolaryngology, Unifesp-EPM.
Study conducted by Federal University of São Paulo - Escola Paulista de Medicina.
Presented at II Congresso Triológico de Otorrinolaringologia, August 2001, Goiânia.
Address correspondence to: Luiz Henrique Fonseca Barbosa - Rua Loefgreen, 1654 ap. 81, Vila Clementino - São Paulo - CEP 04040-002 - e-mail: Luizhenrique.otor@epm.br


