INTRODUCTIONThe mouth-breather syndrome is frequent in childhood, and may be characterized by fatigue, daytime drowsiness, adynamia, poor appetite, nighttime enuresis, and impaired learning and attention. These symptoms result from upper airway obstruction,1 which may often result in dentofacial deformities.2
Mouth breathing is also a risk factor for dental caries and periodontal disease.3,4 The precise mechanisms are not fully understood, but probable causes are gingival surface dehydration, decreased epithelial resistance to bacterial plaques, and lack of salivary auto-cleaning.5 Orthodontic appliances increase the risk of dental caries and gingivitis.6
Although some authors have recognized that oral health has improved in the past few decades,7,8 dental caries remain a serious public health issue not only in Brazil, but in most of the world.10,11 Studies have assessed dental caries calibration and enamel decalcification12-14 based on World Health Organization criteria, such as examining the lesions at initial phases to yield reliable and accurate results for reporting purposes. There are few studies evaluating the potential for caries in high-risk subjects - such as mouth breathers - using fixed orthodontic/orthopedic appliances. These variables may alter the occurrence and severity of caries and periodontal disease. We underline the importance of a multidisciplinary approach for treating these patients effectively.
Thus, the purpose of this study was to conduct a clinical experimental prospective cross-sectional study to assess quantitatively the degree of mineralization of dental enamel and the cariogenic microbiota of mouth breathers that were using fixed maxillary dysjunction appliances.
MATERIAL AND METHODSThe institutional review board of the institution in which the study was carried out evaluated and approved the study project.
1. Sample: there were 20 patients of both sexes, aged from 9 to 13 years, mouth breathers with at least one of the following respiratory conditions: allergic rhinitis, adenoid hyperplasia, palatine tonsil hyperplasia, or nasal septal deviation. All patients had maxillary atresia for which orthodontic/orthopedic maxillary dysjunction was indicated. Patients who had previously been treated orthodontically or orthopedically were excluded. During this study, sample patients were monitored otorhinolaryngologically at the ENT Department of the institution, although still mouth breathing throughout the study period. Clinical dental treatment was also given during orthodontic therapy to improve and adapt mouth conditions in this group of patients.
2. Measuring the degree of mineralization of dental tissues: a Diagnodent® (Kavo, Germany) 1 mW emitting power / 655 nm wavelength / 0 to 99 fluorescence intensity laser diode device was used. The caries detection method with the 655 nm laser diode fluorescence technique measures the amount of demineralization of dental tissues (enamel and dentin); in such cases, organic matter increases and mineral content decreases in these tissues - the fluorophores in organic portions fluoresce. We measured the vestibular surfaces, neck, middle and incisive portions of upper central incisives, and the neck, middle and occlusal portions of the upper first molars before placing and after removing a maxillary dysjunction appliance. The clinical parameters for the DIAGNOdent® are provided as a reference, according to the degree of mineralization, with sensitivity and specificity values.
3. Qualitative bacteriological tests of dental caries: samples of saliva were collected at two times; before installing the maxillary dysjunction appliance, and just before its removal. Patients were asked to eat nothing for two hours, not to perform oral hygiene, and then to produce saliva (non-stimulated) and spit into a sterile universal sample collector. The first pipette was inoculated with 200 µml of saliva, which was dissolved in No Caries® 1. The second pipette was inoculated with 200 µml of saliva, which was dissolved in No Caries® 2. The test tubes were shaken for 15 seconds and placed in an incubator at 37º during 60 minutes. The results were interpreted using a colorimetric reaction scale. Yellow means a NEGATIVE potential for caries, orange means positive (+) that the manufacturer considers as carrying an AGGRESSIVE potential for caries, and pink means positive (++) that the manufacturer considers as VERY AGGRESSIVE potential for caries.
4. Maxillary dysjunction appliance: a Morelli Hyrax-type maxillary dysjunction appliance with an 0.8 mm expanding screw and cemented bands with glass ionomer cement (Sci Farm, USA) with gradual fluoride release was used.
5. Statistics: The numerical values - degree of mineralization - were compared by applying the "t" test for paired samples at a 5% significance level. The cariogenic potential was distributed by incidence.
RESULTSThe "t" test revealed significant differences in the degree of mineralization of dental enamel values before and after the maxillary dysjunction appliance (p=0.0046). Variations in the standard deviation suggested that the sample became less homogeneous at the second study point. Minimum amplitude values remained close, whereas maximum amplitude values increased, which indicated dispersion of values towards the end of orthodontic therapy. The degree of mineralization values gathered at the end of the study ranged from 2.11 to 4.05, with a mean value of 3.08. Table 1 shows the descriptive analysis, and Chart 1 shows the sample behavior.
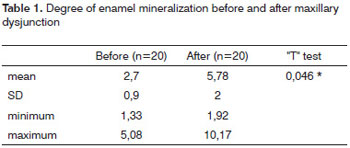
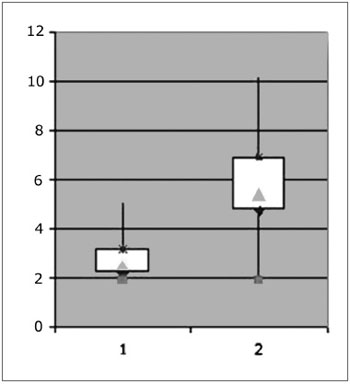
Chart 1. Behavior of the sample before and after maxillary dysjunction.
Salivary bacteriological qualitative measurement data were tabulated; the colorimetric test showed that the potential for dental caries decreased in 45% of the sample, it remained unaltered in 40% of the sample, and increased in only 15% of the sample - Chart 2.
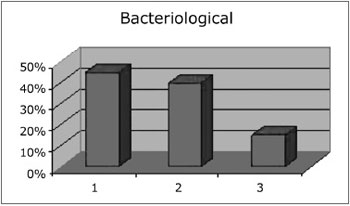
Chart 2. Potential of dental caries before and after the maxillary dysjunction appliance.
Placing orthodontic appliances in the mouth - such as a Hyrax-type dysjunction appliance - may affect the physical, chemical and biological features of the mouth and the bacterial plaque, which may increase caries and periodontal disease.15
The dysjunction appliance in mouth breathers increased significantly the degree of enamel demineralization in our sample; the mean value was 3.08. Based on the reference clinical parameters,16 values from 0 to 5 are within normal limits; these values, therefore, may be considered as "HEALTHY" in histology, not requiring any intervention. Well-adapted appliances and latest-generation cement with gradual fluoride release, and concerns with motivating patients to practice oral hygiene may have minimized possible decalcification.
Saliva diagnosis with No Caries 1 and 2 evaluated the pH and the microbiological aspects. The presence of microorganisms in saliva revealed its status at the collection time and vulnerability even when clinically no caries or gingivitis was seen. The principle of the No Caries test is based on an in vitro reaction by
Streptococcus Mutans and
Neisseria Bucalis, which alter the pH in the solution and change its color by hydrolyzing substrates.17,18
The response to a cariogenic environment varies considerably among individuals; the presence of the maxillary dysjunction appliance increased the potential for caries in only 15% of the sample. These patients were probably less receptive to oral hygiene orientations, which were reiterated in every visit. The 45% that reduced the potential for caries, and the 40% in which this potential remained unchanged regardless of the appliance, possibly because of the knowledge that they would be tested, were induced to perform adequate self-care.
It should be noted that caries do not develop in the absence of dental plaques or fermentation of diet carbohydrates; it may be considered as a diet-bacterial disease.19 Several microorganisms in dental plaques may cause caries, such as
Streptococcus mutans, Streptococcus sobrinus, some lactobacilli species, species of Actinomyces
, Streptococcus nonmutans, and other fermenting bacteria. The caries-associated microbial virulence strongly associated with caries includes the ability to produce acids and to maintain a low pH, which results in dental demineralization.
Streptococcus mutans has all these features, thus its etiological role in caries.19 The presence of a fixed dysjunction appliance makes hygiene more difficult, but not impossible. Therefore, frequent visits from members of a multidisciplinary team - Otorhinolaryngology (assessing upper airways) and Dentistry (hygiene and diet orientations, bacterial plaque prevention, well-adapted and cemented appliances) - were essential for the results of this study.
CONCLUSION1. There was a statistically significant difference in the degree of dental enamel mineralization in mouth breathers after using the maxillary dysjunction appliance; it remained, however, within the normal clinical range.
2. The potential for dental caries increased during orthodontic therapy in a few patients.
3. A multidisciplinary approach contributed to microbiologic dental caries control in mouth breathers.
REFERENCES1. Houve diferença estatisticamente significante no grau de mineralização do esmalte dentário nos pacientes respiradores orais, após a utilização de disjuntor, porém dentro da faixa de normalidade clínica.
2. Um número pequeno de pacientes aumentou o potencial cariogênico durante o tratamento ortodôntico.
3. A abordagem multidisciplinar contribuiu para o controle microbiológico cariogênico do respirador oral.
REFERENCIAS BIBLIOGRÁFICAS1. Di Francesco RC, Passerotii G, Paulucci B, Miniti A. Respiração oral na criança: repercussões diferentes de acordo com o diagnóstico. Rev Bras Otorrinolaringol. 2004;70(5):665-70.
2. Ricketts RM. Respiratory obstruction syndrome. Am J Orthod. 1968;54(7):495-507.
3. Wagaiyu EG, Ashley FP. Mouthbreathing, lip seal and upper lip coverage and their relationship with gingival inflammation in 11-14 year-old schoolchildren. J Clin Periodontol. 1991;18(9):698-702.
4. Nascimento Filho E, Mayer MPA, Pontes PAL, Pignatari ACC, Weckx LLM. A respiração bucal é fator de risco para cárie e gengivite. Rev Bras Alergia Imunopatol. 2003;26(6):243-9.
5. Carranza FA, Hogan EL. Gengival enlargment. In: Newman M, Takei HH. Carranza`s clinical periodontology. 9th ed. Philadelphia: Saunders; 2002. p. 279-96.
6. Heintze SD. A profilaxia individual em pacientes com aparelhos fixos: recomendações para o consultório. Ortodontia. 1996;29(2):4-15.
7. Weyne SC. A construção do paradigma de promoção de saúde: um desafio para as novas gerações. In: Krieger L, coordenador. Promoção de saúde bucal. São Paulo: Artes Médicas; 1997. p. 1-26.
8. Pinto VG. Saúde bucal coletiva. 4a ed. São Paulo: Santos; 2000.
9. Brasil. Ministério da Saúde. Projeto SB Brasil 2003: condições de saúde bucal da população brasileira 2002- 2003 - resultados principais. Brasília: Ministério da Saúde; 2004.
10. Loretto NRM, Seixas ZA, Jardim MC, Brito RL. Cárie dentária no Brasil: alguns aspectos sociais, políticos e econômicos. Rev ABO Nac. 2000;8(1):45-9.
11. Ribeiro AG, Oliveira AF; Rosenblatt A. Cárie precoce na infância: prevalência e fatores de risco em pré-escolares, aos 48 meses, na cidade de João Pessoa, Paraíba, Brasil. Cad Saúde Pública. 2005;21(6):1695-700.
12. Fyffe HE, Deery C, Nugent ZJ, Nuttall NM, Pitts NB. Effect of diagnostic threshold on the validity and reliability of epidemiological caries diagnosis using the Dundee Selectable Threshold Method for caries diagnosis (DSTM).Community Dent Oral Epidemiol. 2000;28(1):42-51.
13. Assaf AV, de Castro Meneghim M, Zanin L, Tengan C, Pereira AC. Effect of different diagnostic thresholds on dental caries calibration - a 12 month evaluation. Community Dent Oral Epidemiol. 2006;34(3):213-9.
14. Assaf AV, Meneghim Mde C, Zanin L, Cortelazzi KL, Pereira AC, Ambrosano GM. Effect of different diagnostic thresholds on dental caries calibration. J Public Health Dent. 2006 Winter;66(1):17-22.
15. Lascada CE, Belluzzo RHL, Lascada Júnior NT. Procedimentos de motivação e higiene bucal em pacientes sob tratamento ortodôntico objetivando a saúde periodontal. Periodontia. 1996;5(4):324-7.
16. Lussi A. Comparison of different methods for the diagnosis of fissure caries without cavitation. Caries Res. 1993;27(5):409-16.
17. Sampaio TPD, Padilha WWN, Lira CC, Leite JCL, Santos Filho L. Reprodutibilidade de teste salivar para microbiota cariogênica. Pesqui Bras Odontopediatria Clín Integr. 2003;3(2):65-9.
18. Pinelli C, Serra MC, Loffredo LC. Efficacy of a dip slide test for mutants streptococci in caries risk assessment. Community Dent Oral Epidemiol. 2001;29(6):443-8.
19. Zero DT. Dental caries process. Dent Clin North Am. 1999;43(4):635-64.
1. Doctoral degree in Sciences, UNIFESP. Professor of the Specialization Orthodontics Course, FAPI
2. Doctoral degree in Sciences, UNIFESP-EPM. Adjunct professor of the Dentistry Course, Feira de Santana State University
3. Specialist in Pediatric Dentistry, volunteer dentist at the Mouth-Breather Unit (Centro do Respirador Bucal), Pediatric ENT Department, UNIFESP
4. Doctoral degree in Sciences, UNIFESP. Professor at the APCD
5. Doctoral degree, head of the Pediatric ENT Discipline, UNIFESP-EPM
6. Full professor in the Pediatric ENT Discipline, Otorhinolaryngology and Head & Neck Department, UNIFESP-EPM, Coordinator of the graduate program of the Otorhinolaryngology and Head & Neck Department, UNIFESP-EPM
Paper submitted to the BJORL-SGP (Publishing Management System - Brazilian Journal of Otorhinolaryngology) on December 8, 2009;
and accepted on March 15, 2010. cod. 6828


