INTRODUCTIONNecrotizing sialometaplasia (NS) is a rare inflammatory disease that normally affects minor salivary glands of the hard palate. It is clinically important because it may simulate malignant neoplasias, such as mucoepidermoid and epidermoid carcinomas1, 2. However, the main evidence of its benign nature is spontaneous evolution to cure, normally between 3-4 and 12 weeks, besides absence of recurrence3, 4.
We have recently seen a case of necrotizing sialometaplasia in a 70-year-old female patient and we decided to report it owing to its rarity and the atypical presentation, which was cystic form on the floor of the mouth. In addition, we would like to attract the attention of surgeons to the fact that although the lesion simulates a malignant entity, it has benign evolution and is cured spontaneously.
LITERATURE REVIEWThe affection was initially described by Abrams et al. in 19735 and is normally presented as an ulcerated nodule on the hard palate and in all regions in which there is a salivary gland6. Its peak of incidence is between the ages of 45 and 55 years, but it has already been described in patients aged 14 to 83 years3. There is no racial predominance and apparently it affects more male than female subjects, with a 2.3: 1 ratio3. Etiology is still unknown but factors such as smoking, alcohol abuse, trauma or even infections have been considered. For most authors3, 4, minor salivary gland infarction seems to be the most probable cause, despite the divergence with other authors.
case reportFemale Caucasian 70-year-old patient, previously healthy, came to the doctor's office complaining of mass on the floor of the mouth for one week, of fast growth, non-painful and without fever or any other associated alteration.
At the physical examination, we detected a hard nodule on the floor of the mouth, in the topography of right sublingual salivary gland, non-elastic and without adherence to profound planes nor ulceration. There were no nodules detected through cervical palpation. Routine laboratory tests did not show any abnormality. The ultrasound test, ordered because of suspicion of salivary duct calculosis, revealed a cystic lesion in the right sublingual salivary gland. Based on this presentation, the patient was submitted to surgery to have the nodule removed. During the surgical procedure, we found a cystic mass, non-encapsulated, hardened and easy to dissect, which affected the topography of the right sublingual salivary gland. The lesion was completely resected and submitted to pathology analysis.
pathology analysis
Macroscopy
Nodular structure of pyramidal format weighing 3g and measuring 3 x 2.2 x 1.3 cm, presenting lobulated external surface, of dark color and cystic consistency. The section surface showed a part of black tissue, apparently hemorrhagic, and a part of dark yellow tissue.
Microscopy
Minor salivary gland presenting cavity recovered by stratified squamous epithelium, without atypia, that contained blood (Figures 1 and 2) close to extensive areas of recent and old hemorrhage amidst fibrous connective tissue, many times hyalinized and containing ducts recovered by stratified squamous epithelium without atypia, surrounded by lymphocytic inflammatory infiltrate (Figure 3). Squamous epithelium formed solid blocks or trabeculae with infiltrative pattern (Figure 4).

Figure 1. Minor salivary gland presenting cavity filled with blood (HE, 32x).
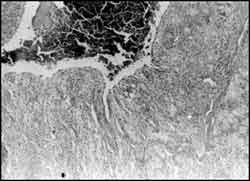
Figure 2. Cavity recovered by stratified squamous epithelium without atypia (HE, 100x).

Figure 3. Duct recovered by metaplastic squamous epithelium on the thickened basal membrane and surrounded by moderate lymphocytic inflammatory infiltrate (HE, 200x).
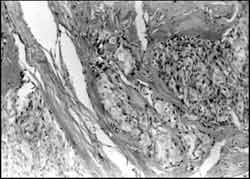
Figure 4. Squamous epithelium without atypia, forming infiltrative blocks and trabeculae; appearance is similar to invasive epidermoid carcinoma (HE, 400x).
Diagnosis: necrotizing sialometaplasia.
The patient presented good postoperative evolution with healing of surgical wound within 30 days. She has been clinically followed up for one year and does not present evidence of recurrence. She only complaints of reduced sensitivity in some regions of the tongue.
DISCUSSIONThis is the report of a case of necrotizing sialometaplasia affecting a sublingual salivary gland of an elderly patient with an atypical presentation of cystic mass. The diagnosis was based on histopathology analysis5, since the clinical findings were not enough to reliably confirm the affection. NS is clinically manifested by profound, non-painful and irregular ulcers, of fast growth, that may extend as far as the bone, simulating squamous carcinoma1, 2, 7. These lesions are frequently recovered by inflammatory or necrotic exsudate, normally surrounded by erythematous halo7. We believe that the cystic presentation of NS reported here is one stage before ulceration, but we do not have enough data to support this hypothesis.
Histologically, we can observe lobules in the seromucous glands with Malpighi metaplasia of canaliculi and adjacent acinus, associated to inflammatory granuloma5. Lobular architecture remains preserved and there are no further cytonuclear atypias. This picture is compatible with what was observed in the present case and demonstrated in Figures 3 and 4.
Most cases described in the literature are located in the minor salivary glands of the hard palate, but there are a number of reports affecting soft palate glands8, retromolar trigonum 8, nasal cavity and nasopharynx9, maxillary sinus10, lower lip11, 12, oral mucosa8, floor of the mouth8, tongue13 and minor salivary glands14, 15. The age of presentation of the nearly 150 cases reported in the literature ranged from 14 to 83 years, and in most patients, the lesion was diagnosed during the 5th and 6th decades of life11. Our patient was older than this age range and the affection was in a minor sublingual gland, a less frequent topography.
NS etiology remains unknown. According to some authors, the initial problem could be vascular16, with ischemia causing salivary lobules necrosis, followed by Malpighi reactional metaplasia, inflammatory reaction and ulceration. The cause of blood supply disorders could be the result of smoking, alcohol abuse, hyperlipidemia, trauma, vascular clamping, embolia, thrombosis, surgical procedures or tumors17. There seems to be a ductal block by nicotine stomatitis or ischemia secondary to arteriolar spasm4, or still the consequence of edema caused by trauma, infection or intra-operative impairment. The reported case had no history of any of these possible risk factors.
The evolution of NS is normally favorable, without recurrence7, and there is no therapeutic recommendation17. Despite the benign characteristics, it is important to always exclude the possibility of squamous carcinoma. For this reason, biopsy is mandatory and it should be large enough for the pathologist to demonstrate the preservation of glandular lobular pattern8. Surgery in such cases has more a diagnostic purpose than a therapeutic one.
closing remarksThe authors emphasized that NS may have atypical presentations and uncommon locations, reason why differential diagnosis with malignant neoplasia is so relevant. Moreover, they stressed the importance of learning more about this affection because, although it is relatively rare, it may cause much suffering and anxiety to patients and family members.
REFERENCES1. Donath K, Seifert G. Tumour-simulating squamous cell metaplasia (SCM) in necrotic areas of salivary gland tumours. Pathol Res Pract 1997;193:689-93.
2. Gilles AD. Necrotizing sialometaplasia. Brit J Oral Surg, 1980;18:4550.
3. Murphy J et al. Necrotizing, sialometaplasia. Oral Surg, Oral Med, Oral Path, 1977;44:419-24.
4. Navarro Sampedro JJ et al. Sialometaplasia necrotizante del paladar duro. Anales ORL Iber-Amer XX, 1993;1:65-77.
5. Abrams AM, Melrose RJ, Howell FV. Necrotizing sialometaplasia: a disease simulating malignancy. Cancer, 1973;32:130-5.
6. Granick MS et al. Necrotizing sialometaplasia masquerading as residual cancer of the lip. Ann Plast Surg, 1988;21:152-4.
7. Gahhos F, et al. Necrotizing sialometaplasia: report of five cases. Plast Reconstr Surg, 1983;71:650-6.
8. Forney SK et al. Necrotizing sialometaplasia of the mandible. Oral Surg, 1977;43:720-9.
9. Maisel RH et al. Necrotizing sialometaplasia involving the nasal cavity. Laryngoscope, 1977;87:429-34.
10. Imbery TA, Edwards P. Necrotizing sialometaplasia: literature review and case reports. J Am Dent Assoc 1996;127:1087-92.
11. Fowler CB, Brannon RB. Subacute necrotizing sialoadenitis: report of 7 cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:600-9.
12. Matilla A et al. Necrotizing sialometaplasia affecting the minor labial glands. Oral Surg, 1979;47:161.
13. Batsakis JG. Tumors of the head and neck, 2d Ed. Baltimore: Williams & Wilkins, 1979;92-4.
14. Batsakis JG. Sialometaplasia. Arch Otolaryngol, 1976;102:191.
15. Bhargova S, Monga JN. Necrotizing sialometaplasia of the parotid. Indian J Cancer, 1975;12:99.
16. Boisnic S et al. La sialométaplasie nécrosante du palais: 3 observations. Ann Dermatol Venereol, 1992;119:922-4.
17. Matsumoto T et al. Necrotizing sialometaplasia in the mouth floor secondary to reconstructive surgery for tongue carcinoma. Acta Pathol Jpn, 1991;41:689-93.
1 Pathologist, Association of Cancer Fight in the Central Area of Brazil, Joint Professor of Endocrinology, Medical School, Triângulo Mineiro (FMTM).
2 Medical School undergraduates, FMTM.
3 Otorhinolaryngologist.
Study conducted at the Medical School, Triângulo Mineiro
Address correspondence to: Dr. Marcus Aurelho de Lima - Disciplina de Endocrinologia - Hospital Escola - Faculdade de Medicina do Triângulo Mineiro
Rua Getúlio Guaritá nº 130 -38028 - 440, Bairro Abadia, Uberaba, MG, Brazil.
Tel: (55 34) 318 5292/5258; Fax: (55 34) 3126640. E-mail: lima@mednet.com.br.
Article submitted on June 29, 2001. Article accepted on August 27, 2001.


