IntroductionChondrosarcoma is a malignant neoplasm of slow growth arising from the cartilaginous tissue. It is not frequently present in the head and neck, being more common in the pelvis, femur, ribs, umerus, scapula, fibula, sacrum and sternal region1.
It is believed that only 10 to 12% of chondrosarcomas are located in the head and neck2 and they comprise only 4% of all non-epithelial nasal cavity, paranasal sinuses and rhinopharynx tumors3. It has greater incidence in male patients at 2:1 ratio, frequently diagnosed around the 3rd and 4th decades of life1, 2. On the face, it is more frequently located on the maxillary bone2, maxillary sinus and more rarely on the septum1. Those located on the temporal bone have longer survival, whereas those located on the maxillary sinus have the worst prognosis2.
CASE REPORTA female patient aged 13 years came to our center complaining of bilateral progressive nasal obstruction for 2 years. There was no history of weight loss, epistaxis, dysphagia, dyspnea and other diseases. One year after the onset of the picture, we noticed facial deformity of the malar region on the right, with strong and sporadic pain. Upon physical examination, in addition to the facial deformity, approximately 3cm in diameter, there was a bulging on the right malar region, observed by a mass occupying the whole right nasal fossa. The tumor was not visualized by anterior rhinoscopy, however, in the nasofibroscopy we could notice a pale mass occupying the whole posterior portion of the left nasal fossa and choana, which deviated the nasal septum and occluded the other choana.
We conducted computed tomography (CT scan) and magnetic resonance imaging (MRI) of the paranasal sinuses. Such exams revealed the presence of a solid mass with bocelated contours in the posterior 2/3 of the nasal septum, maxillary sinus, posterior and anterior ethmoid, sphenoid body and corresponding sinus, in addition to filling completely both choanae (Figures 1 and 2). Together with the sphenoid body on the right, we could notice a solution of contiguity with the cavernous sinus. There were also amidst the solid component some calcifications that corresponded to the cartilaginous matrix. In the MRI, it was not possible to detect invasion of intracranial or other structures (Figure 3).
We decided to conduct a biopsy of the mass that revealed the result of nasal chondroma. Right after the clinical pathology result, we scheduled surgical removal of the tumor, conducted by expanded Caldwell-Luc approach, with complete removal of the mass in fragments. The tumor was medially detached from the septum and the superior-posterior region of the sphenoid. Macroscopically, the tumor had hard consistency and whitish color. After 5 months, we noticed signs of recurrence in the control CT scan and decided to review the clinical pathology analysis. This time, the confirmed diagnosis was grade I chondrosarcoma and we decided to have a new surgical removal of the tumor, removing the medial posterior portion of the nasal septum and detaching the tumor from the lateral wall of the left sphenoid sinus, from the nasal fossa floor on the left and the anterior wall of the maxillary sinus. On the 7th postoperative day we evidenced in the control CT scan a residual lesion in the left sphenoid and posterior-inferior region of the septum (Figure 4 and 5). A last surgical approach was made for the resection of the remaining tumor by endonasal approach.
The patient was asymptomatic after that and in the control CT scan, six months after surgery (Figures 6 and 7), she had not signs of recurrence. Right after the surgery, the patient was referred to radiotherapy and should undergo a new CT scan in 6 months.

Figure 1. Paranasal sinuses CT scan, coronal section, preoperative.

Figure 2. Paranasal sinuses CT scan, axial section, preoperative.
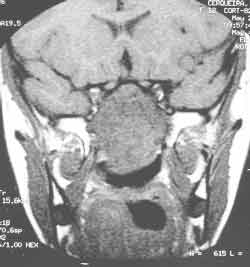
Figure 3. Paranasal sinuses MRI, coronal section, preoperative.

Figure 4. Paranasal sinuses CT scan, coronal section, right after the second surgery.

Figure 5. Paranasal sinuses CT scan, axial section, right after the second surgery.

Figure 6. Paranasal sinuses CT scan, coronal section, control after last surgery.

Figure 7. Paranasal sinuses CT scan, axial section, control after last surgery.
Chondrosarcomas are malignant tumors of slow growth but locally aggressive, which are very prone to recurrence. They amount to 10 to 20% of the primary bone malignant tumors. The main predisposing factors were not found in our patient, which are hereditary multiple exostosis, Ollier's disease and Marfucci's syndrome.2
The case reported here should be highlighted for various reasons. Chondrosarcomas are rare head and neck tumors and even less frequent in women. The clinical picture is variable and can include nasal obstruction, local pain, epistaxis, sinusitis, proptosis, visual blur and headache. Its occurrence in the nasal septum is a rare condition, and there are only 12 cases described in the literature. There is no description of this tumor in a patient as young as ours. It normally affects patients who are aged between 33 and 79 years2.
The diagnosis is given by clinical pathology analysis. Chondrosarcoma characteristics include giant cartilaginous cells with nuclear polymorphism and hyperchromatism 3, comprising multiple nodules that are interconnected with varied sizes. The intercellular space can be of chondroid or mixomatous origin4. The presence of mitosis is not necessary for the diagnosis and calcifications and ossification represent bone erosions and not the production of osteoids by malignant cells. Normally, chondrosarcomas cause local destruction by mass effect before they invade adjacent tissues. Hematogenic dissemination occurs later3. Chondrosarcomas have histology similarities with various other tumors, such as chondromicoid fibroma 5, 6, osteosarcoma, fibrosarcoma 7, chondroma and cordoma 2.
Chondrosarcomas are divided into 3 histology grades (grades I, II and III), according to the level of cell differentiation1, 2, 7, 8. These grades of cell differentiation are classified according to the mitosis rate, cellularity and nuclear size. The patient in question was diagnosed as having grade I chondrosarcoma which may look like benign neoplasm in many situations. This histology type is characterized by small and dense nuclei, intercellular space predominantly chondroid, frequent calcifications and absent mitotic activity 2, 4. In grade II, there are nuclei of greater proportions and moderate size, with small mitosis rate and the intercellular space is normally mixoid. In grade III there are two or more mitosis in ten fields.
The 5-year survival for grades I, II and II is 90%, 81% and 43%, respectively. The 10-year survival drops to 83%, 64% and 29%, respectively. There are no metastases reported in grade I, but grade II and III present rates of 10 and 7%, respectively4.
The prognosis of chondrosarcomas is related to three factors: location, tumor grade and degree of resectability. Among those located in the head and neck, those that are in the nasopharynx and posterior nasal cavity have the worst prognosis, since they can invade the skull base in early stages2, 3, 8. The level of differentiation is also important and the greater the grade, the worse the prognosis2, 8.
The treatment of choice for chondrosarcoma is preferably surgical exeresis in block of the tumor1-3, 8. The patients with paranasal sinuses chondrosarcoma who were submitted to complete resection of the tumor had survival rates ranging from 57 to 62%. It is recommended a minimum follow-up of ten years3. Chondrosarcomas are little radiosensitive and radiotherapy is reserved for cases of recurrence, extensive presentation, high grade or iresectable lesions. Following the example of Princess Margaret Hospital, in which postoperative radiotherapy is reserved for cases of iresectable tumors or margin tumors2. Chemotherapy is a palliative measure for aggressive tumors with local invasion and metastases1.
REFERENCES 1. Finn DG, Goepfert H, Batsakis JG. Chondrosarcoma of the Head and Neck. Laryngoscope December 1984;94.
2. Burkey BB, Hoffman HT, Baker SR, Thorton AF, McClatchey KD. Chondrosarcoma of the Head na Neck; Laryngoscope December 1990;100.
3. Lacovara J, Patherson K, Reaman GH. Primary Nasal Chondrosarcoma. Am J Ped Hematology Oncology 1992;14(2):158-162.
4. Evans HL, Ayala AG, Romsdahl MM. Prognostic factors in Chondrosarcoma of bone. Cancer 1977;40:818-831.
5. Koay CB, Freeland AP, Athansou NA. Chondromixoid fibroma of the nasal bone with extension into the frontal and ethmoidal sinuses. J Laryngol Otol March 1995;109:258-61.
6. Baujat B, Attal P, Racy E, Quillard J, Parker F, Evennou A, Bobin S. Am J Otolaryngol 2001;22:150-153.
7. Koka V, Vericel R, Latigau E, Lusinchi A, Schwaab G. Sarcomas of nasal cavity and paranasal sinuses: chondrosarcoma, osteosarcoma and fibrosarcoma. J Laryngol Otol 1994;108:947-53.
8. Beneck D, Seldman I, Jacobs J. Chondrosarcoma of the nasal septum: A case report. Head and Neck Surgery 1984;7:162-167.
9. Ávalos E, Martín A, Romero L, García D, Martínez E, Araújo J, Albornoz FC. Condrosarcoma nasosinusal. A propósito de un caso. Acta Otorrinolaring Esp 1998;49(8): 245-246.
1 Post-graduate studies, Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
2 Resident Physicians, Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Medical School, University of São Paulo.
3 Ph.D., Professor, Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
4 Associate Professor, Discipline of Otorhinolaryngology, Medical School, University of São Paulo.
Study conducted at the Division of Clinical Otorhinolaryngology, Hospital das Clínicas, Medical School, University of São Paulo
Address correspondence to: Daniel Chung - Av. Dr. Enéas de Carvalho Aguiar, 255 6°andar sala 6021 05403-000 São Paulo SP.
Tel (55 11) 3069-6288 - Fax (55 11) 270-0299
Article submitted on April 30, 2002. Article accepted on June 06, 2002.


