IntroductionIn 1931, Klinger1 described a case of a patient with upper airways disease who died of renal failure. In 1936, Friedrich Wegener2 reported an identical case and, in 1939, he reported a series of cases of the pathology to be known as Wegener's granulomatosis (WG). Fiemberg3, in 1953, introduced together with Carrington and Liebow4 the concept of limited Wegener's granulomatosis. They observed that the disease was restricted to only one or more organs and not necessarily presented involvement of the 3 target-regions (upper airways, lower airways and the kidney). The concept was reinforced by Cassan et al.5.
In 1954, Godman and Churg6 delimited the three classical criteria for diagnosis of Wegener's granulomatosis: the presence of respiratory tract necrotizing granulomatous lesions, vasculitis and glomerulonephritis.
Wegener's granulomatosis is a rare idiopathic systemic disease, immune-mediated, characterized by affecting small arteries of the upper and lower respiratory tract and of the kidneys, leading to inflammatory reaction with necrosis, formation of granuloma and vasculitis in these organs. American studies showed a prevalence of 3 cases for each 100,000 people7, 8. Th mean age at diagnosis is normally between 20 and 40 years and male patients are the most affected ones, in a ratio of 1.5:1.0. It is an uncommon disease in African people9.
The diagnosis is based on clinical picture, clinical pathology of the involved organs and in the positive result of ANCA-c (antinuclear cytoplasmatic antibodies). Treatment is conducted with immunosuppressing drugs and should be started as early as possible since it is a severe pathology that results in death because of the infections and renal failure.
As general initial symptoms, the patients normally manifest fever, anorexia, weight loss, fatigue and weakness9.
The upper respiratory tract is involved in 70 to 100% of the cases. The most frequent manifestations involve the nose and paranasal sinuses (in 80 to 90% of the cases) and they are: chronic nasal obstruction with light rhinorrhea, nasal mucosa edema and ulceration, parosmia, epistaxis and headache. Perforation of nasal septum and ulceration and erosion of the vomer are classical findings. Nasal deformity in saddle, owing to the destruction of the nasal cartilage and vomer, is detected in only 3.5 to 7% of the cases. Such damages are frequently infected secondarily with Staphylococcus aureus7,10,11.
There can be secretory otitis media, chronic otitis media, with tympanic membrane perforation, otalgia and otorrhea. There are cases described of sensorineural hearing loss, vertigo and tinnitus in patients with Wegener's granulomatosis 12.
The prevalence of otological involvement ranges at about 35% and it is related to vasculitis and auditory tube blockage by affecting the rhinopharynx 7, 12.
Facial paralysis is found in 8 to 10% of the cases and results from the vaso-vasorum vasculitis of the facial nerve, or the granulomatous invasion of the middle ear invasion, or the primary granulomatous damage to nerves or the combination of such factors.
Pulmonary involvement is also extremely common (70 to 90% of the cases). Productive cough, dyspnea, hemoptysis, pain and thoracic discomfort, are the main symptoms. Abnormalities in the chest x-rays are seen in over 90% of the cases, including non-calcified excavated nodular damages that are large, multiple and bilateral.
The nephrological characteristics of Wegener's granulomatosis are predominantly represented by focal necrotizing glomerulonephritis, which leads to renal failure and death. Renal abnormalities are found in 50 to 90% of the cases. Hematuria, leukocyturia and abnormal measures of urea and creatinine are abnormalities found in patients' tests.
Skin manifestations (petechia and ulcerated lesions) are detected in approximately 40% of the cases, in the extremities of lower limbs.
Migration myalgia and arthralgia are frequent (40 to 70%), but temporary.
Ocular, heart and central nervous system affections are present in about 40% of the cases and they are nonspecific.
Dysphonia, laryngeal stridor, wheezing, ulceration and oral edema and gingivitis complement the head and neck impairment7.
The golden standard for diagnosis of Wegener's granulomatosis is the detection of necrotizing granulomatous vasculitis at the clinical pathology of the biopsied affected tissue. Necrosis is normally large, with leukocytarian debris and polymorphonuclear micro-abscesses. Granulomatous lesions present polymorphonuclear, plasma cells, rare eosinophils and lymphocytes and, specially, giant multinuclear cells. Vasculitis is characterized by the involvement of arterioles and venules, as a consequence of the vascular lumen occlusion10, 11.
Lung tissue, obtained preferably by open thoracotomy, provides much information to diagnosis, proving to be necrotizing granulomatous vasculitis in most cases10, 11.
The finding of high titles of ANCA-c supports the diagnosis. ANCA-c are circulating antibodies against the elements of neutrophils and monocytes cytoplasmatic nuclei. Indirect immunofluorescence is the best method to titrate ANCA-c. Values higher than 1/16 are considered positive7, 9-11.
Many investigators believe that ANCA-c is highly specific for Wegener's granulomatosis, with 98% specificity and sensitivity that varies from 34 to 92%. However, other authors reported positive responses of ANCA-c in other vasculitis and autoimmune syndromes, such as polyarthritis nodosa and Kawasaki's disease7.
Wegener's granulomatosis is based on clinical history, physical examination findings, radiology, tomography clinical pathology and positive ANCA-c 9, 4.
Positive diagnoses are rarely made in very early forms of WG and in cases of limited WG9.
In a typical manifestation, the classical clinical pathology picture of WG allows immediate differentiation from other disorders, such as polyarthritis nodosa, Churg Strauss syndrome, lymphoma, cocaine abuse, medial-facial granuloma, Goodpasture syndrome, tuberculosis and the other granulomatous diseases9-12.
WG treatment is based on the use of immunosuppressing drugs. It is advocated the use of cyclophosphamide, administered at doses of 2mg/Kg/day PO. Leukocyte count should be monitored closely during therapy, and the dosed adjusted according to the neutrophil count, which should be higher than 3,000mm3. Cyclophosphamide should be continued for one 1 year after the induction of complete remission, and then gradually reduced up to complete withdrawal.
Initially, glucocorticoids can be administered together with cyclophosphamide. In general, we used prednisone 1mg/Kg/day initially (1st month of therapy), followed by a daily regimen, with gradual conversion to an alternate day program, followed by reduction and suspension after 6 months.
Some reports indicate a beneficial effect of the association between sulphamethoxazole-trimethophim to control secondary infections to WG, but there is no concrete evidence to support it, especially in patients with severe renal and pulmonary disease.
The mean survival rate of patients is 8 years and a half; 10-year survival is estimated in 40% if there is involvement of the kidney and in 60 to 70% if there no is renal involvement7.
Case ReportEIP, aged 18 years old, female, Caucasian patient. Two months before she started with frontal and left hemifacial headache, with no irradiation, insidious onset, progressive worsening followed by nasal obstruction, anterior and posterior purulent rhinorrhea, epistaxis, cacosmia, and fever. She came for medical service 5 days later when she was treated with amoxicyllin for 10 days, owing to the suspicion of acute rhinosinusitis. She manifested general worsening of the case, high fever, chest pain, dyspnea, productive cough with greenish expectoration, otalgia, otorrhea and bilateral hearing loss. At the occasion, she came for medical service again and was hospitalized for better assessment and treatment at Hospital Municipal Universitário de São Bernardo do Campo.
She had lost 8 kilos, had asthenia, vertigo and right knee arthralgia. There was no relevant personal or family history.
Upon physical examination, she was pale ++/4, dehydrated +/4, no fever and tachycardia (HR 120 bpm). The otorhinolaryngological examination revealed ample central tympanic membrane perforation bilaterally, abundant otorrhea, deformity of the nasal dorsum in saddle, abundant brown crusts in both nasal fossae, intact nasal septum but showing mucosa of granulous aspect, hypotrophic lower and middle nasal conchae. Mouth and oropharynx had no abnormalities.
Pulmonary auscultation revealed bilateral vesicular murmur, with mild sparse whistles, diffuse cracking stertors and snores, especially on the right hemithorax.
She presented petechiae of the low limbs. The remaining systems were intact.
We ordered complete lab tests to better define the diagnosis, etiology and extension of the disease. Complete blood count showed monocytic normochromic anemia and leukocytosis without deviation on the left (19,500 leukocytes).
Chest x-ray and CT scan presented images that suggested abscess on the middle and upper thirds of the right lung; calcification of the right pulmonary hylus, pneumonic foci on the left and bilateral pleural fluid.
Paranasal sinuses CT scan showed thickening of the nasal fossa mucosa lining; maxillary sinus communication with the nasal cavity bilaterally, hypotrophic inferior and middle nasal conchae, material with soft part density in the maxillary, frontal, ethmoid and sphenoid sinuses (Figures 1, 2, 3 and 4).
BAAR study in sputum was negative in various samples. PPD, HIV serology and FTA-ABS were also negative. Sputum culture was positive for Pseudomonas and negative for fungi. The culture of pleural fluid was negative for BAAR and fungi.
At bronchoscopy, we visualized an ulcerated lesion and extrinsic compression of the right source-bronchium. We conducted a biopsy of the lesion whose clinical pathology showed extensive areas of necrosis and neutrophil exsudate.
Clinical pathology of the biopsy conducted in nasal mucosa presented nonspecific chronic inflammatory process.
ANCA-c titration was positive (1/32).
After positive response of ANCA-c, we decided to conduct a nasal mucosa biopsy but under microscopy to confirm the diagnosis of Wegener's granulomatosis. Clinical pathology showed fragments of respiratory mucosa partially recovered by stratified pavement epithelium, presenting in the chorion numerous small caliper vascular structures, whose walls were filled with neutrophils and eosinophils, plus edema and mixed infiltrate. Some vessels had clear aggression of the walls, with areas of fibrinoid necrosis. The histology suggested necrotizing vasculitis granulomatosis.
Renal function was investigated, checking urea and creatinine doses, whose results were normal. Urine analysis I showed mild micro-hematuria.
Pure tone audiometry detected bilateral mild to severe conductive loss, ascending and symmetrical. There was good vocal discrimination.
The patient presented clinical worsening, with radiographic and tomographic evidence, despite the wide spectrum antibiotic therapy. Many bactericide and bacteriostactic antimicrobials were introduced, considering the clinical picture and the results of complementary tests requested. Ceftriaxone, clindamycin, vancomycin, metronidazole, imipenem, amykacin, tazocin, amphotericin B and triple regimen for tuberculosis were used as a sequence by the clinician to try to control the infectious condition, but unsuccessfully. After the result of Positive ANCA-c and the result of the second nasal mucosa biopsy, we confirmed the diagnosis of Wegener's granulomatosis and started treatment with cyclophosphamide and prednisone. At the beginning of treatment, the patient was submitted to a partial pneumectomy on the right, owing to the massive affection and destruction of the right lung. After the surgery and maintenance of the immunosuppressing drugs, the patient presented significant improvement and was discharged from hospital 15 days later.
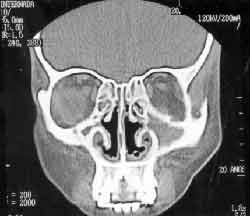
Figure 1. Coronal section, showing affecting of the maxillary and anterior ethmoid sinuses.

Figure 2. Axial section, showing impairment of the maxillary sinuses and nasal fossa.

Figure 3. Axial section, showing impairment of the ethmoid sinuses.

Figure 4. Axial section with frontal impairment.
The patient did not fit the most common profile for suspicion of Wegener's granulomatosis. Even though the clinical picture was suspicion, the fact that she was female and adolescent was conflicting with the literature date.
In the first visit, we thought it were a tuberculosis associated with the second bacterial infection in the upper and lower airways, which was not confirmed by the complementary tests. The introduction of the triple medication for tuberculosis did not affect the course of the disease.
Biopsy of nasal and bronchial tissue were inconclusive and excluded the possibility of having Wegener's granulomatosis at first sight. The fact that the urinary tract was not affected has also contributed to considering this as a less probable diagnosis.
However, after positive response to ANCA-c, we decided for a new nasal biopsy directed by optic microscopy for the extraction of the material that was clearly sick. With the findings of necrotizing granulomatous vasculitis, which is typical of Wegener's granulomatosis, the diagnosis was defined and the immunosuppressing treatment was started, noticing significant improvement of the case.
ConclusionWegener's granulomatosis is a rare entity and making its diagnosis is a real challenge to physicians. The hypothesis should be made when there are symptoms related with upper and lower airways and the kidneys. Our patient, however, had no renal compromise, fitting the concept of limited Wegener's granulomatosis, which contributed to an even more unlikely diagnosis.
The clinical picture had a dramatic progression up to the final diagnosis, leading to partial removal of the right lung which could have been prevented if we had concluded for the disease before.
We suggest that nasal biopsies are conducted under microscopic or endoscopic view, avoiding diagnostic failures because of healthy or insufficient material, which delays substantially the definition of the disease, increasing the sequelae of the granulomatous process.
It is extremely important that the diagnosis is made as early as possible so that immunosuppressing treatment can be started leading to remission, reducing morbidity and mortality of the disease.
References 1. Klinger H. Grenzformen der Periarteritis nodosa. Frankf Z Pathol 1931;42:455-80.
2. Wegener F. Uber generalisierte, septische Gefässerkrankungen. Verh Dtsch Ges Pathol 1936;29:202-10.
3. Fienberg R. Necrotizing granulomatosis and angiitis of the lungs. Am J Clin Pathol 1953;23:413-28.
4. Carrington CB, Liebow M. Limited forms of angiitis and granulomatosis of Wegener's type. Am J Med 1966;41:497-527.
5. Cassan SM, Coles DT, Harisson EG. The concept of limited forms of Wegener's granulomatosis. Am J Med 1970;49:366-79.
6. Godman GC, Churg J. Wegener's granulomatosis. Pathology and review of the literature. Arch Pathol 1954;58:533-53.
7. Hartl DM, Aidan P, Brugière O, Sterkers O. Wegener's Granulomatosis Presenting as a Recurrence of Chronic Otitis Media. Am J Otol 1998;19(1):54-60.
8. Koldingsnes W, Nossent H. Epidemiology of Wegener's Granulomatosis in Nothern Norway. Art Rheum 2000;43 (11):2481-7.
9. Devaney KO, Ferlito A, Devaney SL, Hunter BC, Rinaldo A. ClinicoPathological Consultation: Wegener's Granulomatosis of the Head and Neck. Ann Otol Rhinol Laryngol 1998;107:439-45.
10. Jennings CR, Jones NS, Dugar J, Powell RJ, Lowe J. Wegener's Granulomatosis - A review of diagnosis and treatment in 53 subjects. Rhinology 1998;36:188-91.
11. Jones NS. Nasal manifestations of rheumatic diseases. Ann Rheum Dis 1999;58:589-90.
12. Scully RE, Mark EJ, Mcneely WF, Ebeling SH. Case Records of the Massachussets general Hospital. N Engl J Med 1999;340(17): 1349-53.
1 Resident physician - 3rd year - in Otorhinolaryngology, Medical School, University ABC.
2 Resident physician - 1st year - in Otorhinolaryngology, Medical School, University ABC.
3 Teaching Support, Discipline of Otorhinolaryngology, Medical School, University ABC.
4 Faculty Professor, Discipline of Otorhinolaryngology, Medical School, University ABC.
Discipline of Otorhinolaryngology, Medical School, University ABC - Av. Príncipe de Gales 821 Santo André SP Brazil 09060-650 - Tel (55 11)449-3347
Address correspondence to: Rubens E. C. Rodrigues - Rua Estrada Velha da Penha 88 apto 72 bloco 2, 03090-020 Tatuapé São Paulo SP.
Article submitted on February 28, 2002. Article accepted on March 28, 2002.


