INTRODUCTIONSnoring and obstructive sleep apnea are very common in the general population and usually happen because of a partial or total collapse of the upper airways during sleep1. Upper airway segments responsible for airflow resistance during sleep involve the nasal cavities (such as nasal conchae hypertrophy, septum deviation and polyps), the rhinopharynx (adenoid hypertrophy and flaccid palate), the oropharynx (lateral pharynx wall hypertrophy and large uvula, palatine tonsils hypertrophy or lingual tonsil hypertrophy); or pharyngeal-Larynx (tumors and malacia), representing different places of obstruction. Assessment by indirect nasal-pharyngoscopy is carried out routinely, because these anatomical alterations are responsible for an increase in airflow resistance and are potentially correctable by surgery.
The obstruction functional or dynamic components are represented by collapse and pharyngeal walls narrowing or vibration during sleep, and may be more evident in isolate or multiple segments (retropalatal and/or retrolingual regions). Muscle tone, airway inner diameter, fat deposits and cranial-facial bone shape, all influence the degree of obstruction in these segments of the soft pharynx, which do not have bone or cartilage support2-4. In these matters, the nasal-pharyngoscopy with Müller's maneuver (which assesses the dynamic behavior and the degree of retropalatal and retrolingual collapse during maximum inspiration with both the mouth and he nose occluded) is the assessment method currently being used5. Nonetheless, its usefulness in surgery planning with the goal of correlating its findings with the success expectations of surgical treatment (especially, uvulopalatopharyngoplasty - UPPP) is extremely controversial6-8. There are some papers, which correlate retropalatal collapse alone with the therapeutic success of UPPP for the treatment of OSAS, and others did not find this correlation9,10.
There are numerous potential limitations associated with Müller's maneuver: it assesses the upper airways during the day, while obstruction happens during sleep. Another limitation is that most of the studies do not quantify the negative pressure generated by the patient during Müller's maneuver. In order to reduce these biases, some studies with videonasal-laryngoscopy under sleep induction have been carried out since 199011,12. These studies show differences between obstruction sites (retropalatal and retrolingual) observed during Müller's maneuver13,14 and during induced sleep, suggesting that this last one would be the method closer to what really happens during sleep.
The goal of the present investigation was to describe an anatomical and functional method (comparing the upper airways gauge variation in the retropalatal and retrolingual areas) through induced sleep and compare it to Müller's maneuver carried out with the patient awake.
MATERIALS AND METHODSThis research protocol (# 370/03) was approved by the Ethics Committee of our institution.
We studied 8 patients (3 men and 5 women), at the ages of (mean ± standard deviation) 48.6 ± 9.2 years and body mass index (BMI) of 26.6± 5.7 kg/m2 with clinical history of loud snoring. All the patients went through videonasal-pharyngoscopy by means of an OlympusR video bronchoscope of 4.9mm of external diameter. No topical anesthesia on the oropharynx or larynx was used. We used 2% lidocaine gel for nasal lubrication, facilitating the scope's passage.
Videonasal-pharyngoscopy was carried out with the patients laying down on dorsal decubitus, with peripheral venous punction and monitoring. We did photographic documentation in three consecutive stages:
a) anatomical evaluation of the nose, pharynx and larynx;
b) Müller's maneuver with the patient awake, in dorsal decubitus, measuring inspiratory pressure by means of a manovacuometer coupled to the bronchoscope's working port (Figure 1);
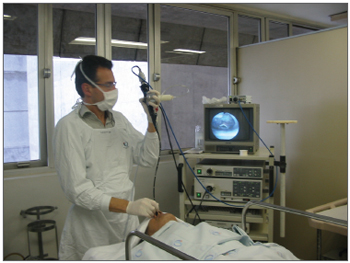
Figure 1. Müller's maneuver through intermittent nasal occlusion and maximum inspiration. We used a manovacuometer for pressure recording.
c) induced sleep. Müller's maneuver was based on creating negative pressure through vigorous inspiration having both the nose and the mouth occluded. We considered the maneuver to be effective only when the patient reached the negative pressure of 40 cm/H2O 14,15. For this maneuver we positioned the video bronchoscope in two different levels: at the rhinopharynx and at the oro-pharyngeal transition site, allowing us to quantify the collapse in these two levels, according to the description below. After Müller's maneuver, we induced the patient's sleep by dripping 10mg of midazolam diluted in 100mL of saline solution in the burette. We interrupted the endovenous infusion as soon as the patient slept - easily noticed after he/she started snoring. During induced sleep, we positioned the video bronchoscope in the same regions where we monitored the Müller's maneuver (retropalatal and retrolingual). We monitored the patients by continuously recording their breathing by means of a nasal flow sensor (pressure canula), respiratory effort (thoracic-abdominal band) and pulse oxymeter (Stardust, RespironicsR device) during videonasal-pharyngoscopy, and for 15 minutes after removal of the fiberscope. These exams were carried out in the bronchoscopy room, equipped with material for intubation, mechanical ventilation and emergency care. Data obtained by polysomnography during videonasal-pharyngoscopy were later compared with those from the conventional polysomnography, and this comparison will be published later.
The obstruction of the regions studied, both during Müller's maneuver, as well as during induced sleep, was measured in a semi-quantitative fashion in: no obstruction (0) or up to 25% obstruction (1), 50% (2), 75% (3) and 100% (4) of obstruction. (Chart 1)
We used the Mann-Whitney Rank Sum Test (SigmastatÒ 3.1) in order to compare retropalatal and retrolingual obstruction seen during Müller's maneuver and during induced sleep.
RESULTSEndoscopic anatomical evaluation showed nasal conchae hypertrophy in six of the eight patients (75%) and nasal septum deviation in four of the eight (50%). We did not see other anatomical alterations, including adenoid or tonsil hypertrophy, tumors or malformations. Midazolam dose for sleep induction varied from 4 to 10mg (mean value of 6.1 + 2.1). All patients awoke spontaneously after the study - it was not necessary to use drugs for pharmacological reversion.
Obstruction levels we saw during Müller's maneuver and induced sleep were of mean + standard deviation 3.13 + 0.99 and 2.75 + 0.46, respectively, p= 0.234 (Graph I). In contrast, retrolingual obstruction was significantly less during Müller's maneuver (mean + standard deviation 0.63 + 1.06 and 2.63 + 1.30, respectively, p= 0.005) (Graph II). Figure 2 shows respiratory monitoring during induced sleep of a patient who presented with severe obstructive sleep apnea. Monitoring showed that the respiratory events during induced sleep were obstruction-related (that is: there was inspiratory effort detected by the chest-band during breathing). The lower saturation observed was of 85%, present during obstructive events. No patient required oxygen complementation or sleep interruption because of prolonged apnea.
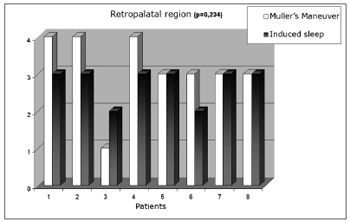
Chart 1. Retropalatal region collapse estimated by Müller's maneuver and induced sleep.
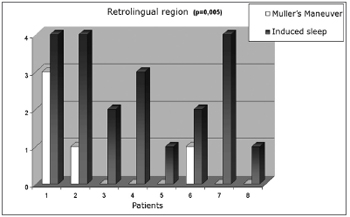
Chart 2. Retrolingual region collapse estimated by Müller's maneuver and induced sleep.
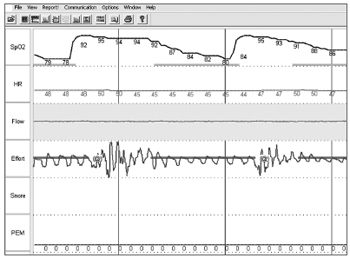
Figure 2. Polysomnography during nasal endoscopy under induced sleep.
Our investigation described the videonasal-pharyngoscopic evaluation of the upper airway, in a sequential manner, allowing for diagnoses of structural (anatomical alterations) and functional disorders during the patients waking hours, by means of the Müller's maneuver and during sleep induced by midazolam. While retropalatal obstruction was common with the two maneuvers, during induced sleep we noticed more retrolingual obstruction than Müller's maneuver with the patient awake. Thus, these data suggest that Müller's maneuver can underestimate retrolingual collapse. Midazolam-induced sleep may become an important tool in assessing the upper airway obstruction site, and in the future it may help in the therapeutic choice for these patients with snoring, in whom we suspect of sleep obstructive apnea syndrome.
On the way between the choanas and the hypopharynx, the retropalatal and retrolingual regions are the ones most prone to collapse16, since they are narrow and do not have a bony or cartilaginous support framework. Therefore, these regions seem to be the primary site responsible for partial collapse, causing snoring. Total collapse causes obstructive sleep apnea. Intra-thoracic negative pressure und resistance (Müller's maneuver), associated with nasal-laryngoscopy, allows for a dynamic evaluation of upper airway collapse in the entire pharynx.17 Some studies consider Müller's maneuver a key point in the functional pre-operative assessment for uvulopalatopharyngoplasty in patients with snoring and/or obstructive sleep apnea syndrome. Müller's maneuver has been used in the clinical practice not only to locate and classify retropalatal and retrolingual obstruction, but also to aid in surgical decision making. Obstruction alone has been considered a success factor for uvulopalatopharyngoplasty. Nonetheless, this concept has been broadly challenged, as well as the usefulness of traditional approaches18. Assessing the laxity of the entire larynx by means of the Müller's maneuver has contributed to the planning of different palatal pharyngoplasties; however its role in locating the site of obstruction must be revised, since its quantification is not correlated with OSAS, nor with the results of different surgical treatments.19,20 In greater or lesser degrees, OSAS must be considered a disease that involves the entire pharynx. In this context, we believe that the induced sleep method proposed in the present investigation may become an important tool to aid in this surgical approach.
In our small sample of patients, we found nasal alterations in a great number of patients. Nasal disease must be better described during the initial nasal endoscopy exam, in order to provide data regarding the degree of airflow obstruction. Nasal disease is common in the general population and it may play a role in pharyngeal obstruction in patients with sleep obstructive apnea syndrome21-23. Some authors suggest that nasal obstruction usually plays a role in the so called "oral breather", in whom there is a posterior shift of the tongue and mandible, reducing the airway gauge and altering the efficacy of pharyngeal dilating muscles (predisposing the patient to collapse during sleep). These factors, associated with obesity, soft tissue hypertrophy (pharyngeal lateral walls) and cranial-facial structural alterations play a role in the obstruction of collapse-susceptible regions and increase in respiratory effort.
Our study included the measurement of the negative pressure generated by the patient during Müller's maneuver, by means of a manovacuometer coupled to the working port of the videobronchoscope (Figure 1). Thus, we selected only the maneuvers that created significant effort (Pressure >40 cm H2O). This is a low cost methodology that is not routinely used and could be easily added to the method. In fact, we observed that many patients had to have the maneuver repeated many times before we could reach an acceptable minimal pressure. Most of the papers published so far did not use any type of objective measurement of the negative pressure created by the patient during Müller's maneuver. This limitation to the method may contribute to explain the disagreeing results among studies.
Because of the limitations and controversies related to the real usefulness of laryngoscopy in waking patients, many authors advocate the idea that induced sleep could be a more accurate method to quantify and locate the point of collapse in the upper airway (UAW).24-26 For example, a prospective and controlled study14 which induced sleep with titrated doses of propafenone (propofolR) and evaluated UAW behavior in a group of patients with apnea showed that this method was safe, specific and sensitive. In our study we used a methodology similar to the one described by Sadaoka et al.27 and we induced sleep with low doses and slow dripping of midazolam, acting only as a sleep inducer and not as a sedative agent. We showed that the method is safe, and during the procedure the patients could wake up at any time. All patients woke up spontaneously after the test, without the need to use antagonist agents. Despite all of this, we highlight the importance of employing this method in a place that has the means for oro-tracheal intubation, mechanical ventilation and post-procedure observation should it be necessary. Midazolam has the advantage of being inexpensive and more readily available than propofol. In our country, to use propofol one needs to have an anesthesiologist to help, and this increases costs. In our study, nasal endoscopy with induced sleep was followed by respiratory monitoring in real time and allowed us to document the fact that the apneas seen were indeed obstructive (Figure 2).
CONCLUSIONThis study opens an important perspective in the preoperative endoscopic assessment of patients with snoring and obstructive sleep apnea, and we concluded that this estimate of the obstruction level by induced sleep is better than Müller's maneuver.
REFERENCES1. Schwab RJ. Upper airway imaging. Clin Chest Med 1998;19(1):33-54.
2. Wilms D, Popovich J, Conway W, Fujita S, Zorick F. Anatomic abnormalities in obstructive sleep apnea. Ann Otol Rhinol Laryngol 1982;91(6 Pt 1):595-6.
3. Hudgel DW. The role of upper airway anatomy and physiology in obstructive sleep apnea. Clin Chest Med 1992;13(3):383-98.
4. Badr MS. Pathophysiology of upper airway obstruction during sleep. Clin Chest Med 1998;19(1):21-32.
5. Sher AE, Thorpy MJ, Shprintzen RJ, Spielman AJ, Burack B, McGregor PA. Predictive value of Müller maneuver in selection of patients for uvulopalatopharyngoplasty. Laryngoscope 1985;95(12):1483-7.
6. Skatvedt O. Localization of site of obstruction in snorers and patients with obstructive sleep apnea syndrome: a comparison of fiberoptic nasopharyngoscopy and pressure measurements. Acta Otolaryngol 1993;113(2):206-9.
7. Katsantonis GP, Maas CS, Walsh JK. The predictive efficacy of the Müller maneuver in uvulopalatopharyngoplasty. Laryngoscope 1989;99(7 Pt 1):677-80.
8. Aboussouan LS, Golish JA, Wood BG, Mehta AC, Wood DE, Dinner DS. Dynamic pharyngoscopy in predicting outcome of uvulopalatopharyngoplasty for moderate and severe obstructive sleep apnea. Chest 1995;107(4):946-51.
9. Petri N, Suadicani P, Wildschiodtz G, Bjorn-Jorgensen J. Predictive value of Müller maneuver, cephalometry and clinical features for the outcome of uvulopalatopharyngoplasty. Evaluation of predictive factors using discriminant analysis in 30 sleep apnea patients. Acta Otolaryngol 1994;114(5):565-71.
10. Doghramji K, Jabourian ZH, Pilla M, Farole A, Lindholm RN. Predictors of outcome for uvulopalatopharyngoplasty. Laryngoscope 1995;105(3 Pt 1):311-4.
11. Pringle MB, Croft CB. A comparison of sleep nasendoscopy and the Müller manoeuvre. Clin Otolaryngol Allied Sci 1991;16(6):559-62.
12. Croft CB, Pringle M. Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci 1991;16(5):504-9.
13. Pringle MB, Croft CB. A grading system for patients with obstructive sleep apnoea--based on sleep nasendoscopy. Clin Otolaryngol Allied Sci 1993;18(6):480-4.
14. Steinhart H, Kuhn-Lohmann JC, Gewalt K, Constantinidis J, Mertzlufft F, Petak M, et al. [Pharyngolaryngoscopic findings in patients with obstructive sleep apnea syndrome and primary snoring]. Hno 2000;48(12):917-21.
15. Ritter CT, Trudo FJ, Goldberg AN, Welch KC, Maislin G, Schwab RJ. Quantitative evaluation of the upper airway during nasopharyngoscopy with the Müller maneuver. Laryngoscope 1999;109(6):954-63.
16. Schwab RJ. Pro: sleep apnea is an anatomic disorder. Am J Respir Crit Care Med 2003;168(3):270-1.
17. Strohl KP. Con: sleep apnea is not an anatomic disorder. Am J Respir Crit Care Med 2003;168(3):271-2.
18. Terris DJ, Hanasono MM, Liu YC. Reliability of the Müller maneuver and its association with sleep-disordered breathing. Laryngoscope 2000;110(11):1819-23.
19. Cahali MB, Formigoni GG, Gebrim EM, Miziara ID. Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep 2004;27(5):942-50.
20. Woodson BT. A piece of the surgical puzzle. Sleep 2004;27(5):844-6.
21. Figueiredo ACd, Lorenzi MC, Prezzoti S, Cabral MM, Sennes LU, Lorenzi-Filho G. Efeitos da pressão positiva contínua em vias aéreas sobre os sintomas nasofaríngeos em pacientes com a síndrome da apnéia obstrutiva do sono [Effects of continuos positive airway pressure on nasal and pharyngeal symptoms in patients with obstructive sleep apnea]. J Pneumol 2004;30:535-9.
22. Rappai M, Collop N, Kemp S, deShazo R. The nose and sleep-disordered breathing: what we know and what we do not know. Chest 2003;124(6):2309-23.
23. Chen W, Kushida CA. Nasal obstruction in sleep-disordered breathing. Otolaryngol Clin North Am 2003;36(3):437-60.
24. Marais J. The value of sedation nasendoscopy: a comparison between snoring and non-snoring patients. Clin Otolaryngol Allied Sci 1998;23(1):74-6.
25. Abdullah VJ, Wing YK, van Hasselt CA. Video sleep nasendoscopy: the Hong Kong experience. Otolaryngol Clin North Am 2003;36(3):461-71.
26. Berry S, Roblin G, Williams A, Watkins A, Whittet HB. Validity of sleep nasendoscopy in the investigation of sleep related breathing disorders. Laryngoscope 2005;115(3):538-40.
27. Sadaoka T, Kakitsuba N, Fujiwara Y, Kanai R, Takahashi H. The value of sleep nasendoscopy in the evaluation of patients with suspected sleep-related breathing disorders. Clin Otolaryngol Allied Sci 1996;21(6):485-9.
1 PhD, Assistant physician at the Respiratory Endoscopy Service of the University of São Paulo Medical School.
2 PhD, Assistant physician at the Respiratory Endoscopy Service of the University of São Paulo Medical School.
3 PhD Student, Pneumology - University of São Paulo Medical School - Polysomnography technician - Instituto do Coração, INCOR.
4 PhD. Assistant at the Department of otorhinolaryngology - University of São Paulo Medical School.
5 PhD. Head of the Department of Pneumology of the Fleury Laboratory.
6 Associate Professor, Head of the Sleep Laboratory - Incor, Discipline of Pneumology - Department of Cardio-Pneumology.
University of São Paulo Medical School - Hospital.
Send correspondence to: Av. Dr. Arnaldo, 455 - Cerqueira César 01246-903 São Paulo SP.
Tel. (0xx11) 3069-7251 / 3069-7244 - Serviço de Broncoscopia.
Paper submitted to the ABORL-CCF SGP (Management Publications System) on February 7th, 2006 and accepted for publication on March 13th, 2006. cod. 1713.


