INTRODUCTIONMadelung's disease, also known as Multiple Symmetric Lipomatosis (MSL), Benign Symmetric Lipomatosis, or Adenolipomatosis of Lanouis-Bernard is a benign rare entity of unknown etiology, clinically characterized by depositions of multiple non-encapsulated fatty tissue located on the neck and upper trunk regions and symmetrically distributed1, 2.
It was initially reported by Benjamin Brodie (1846), who described the patient that presented accumulation of fatty tissue on the submentoneal. retroauricular and neck regions, with symmetrical and annular disposition. In 1888, Otto W. Madelung, in a study involving 33 patients, reported the classical cervical lipomas horse collar distribution 3-5. In 1898, in an extensive review of 65 patients, Launois and Bensaude completed the description of the syndrome characterizing it as different and little disseminated, having as the main characteristics the formation of diffuse and symmetrical fatty deposits on the neck region6, 7, 8.
There are only 200 cases reported in the literature. It is more frequent in adult males, alcohol abusers who live in Mediterranean countries, with possible autossomal dominant heredity. It is rare in women and non-abusers of alcohol7, 9, 10.
It is frequently associated with systemic abnormalities such as liver pathology, intolerance to glucose, diabetes mellitus, blood hypertension, hyperlipoproteinemia, hyperuricemia, hypothyroidism, macrocytic anemia, polyneuropathy, acute tubular acidosis and malignant upper airway tumors7, 9. Surgical excision is the only confirmed effective treatment approach, but recurrences are frequent3. In the present study, the authors described 3 cases of Madelung's disease and reviewed the literature emphasizing epidemiology, etiopathogenesis, clinical picture, treatment and prognosis.
CASE REPORTThree male Caucasian patients respectively aged 45, 48 and 55 years, living in the state of São Paulo, were treated at Núcleo de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço de São Paulo, between 1987 and 1997, presenting symmetrical accumulation of fatty tissue on the neck and thoracic regions.
They reported onset of the lipoma in adult life, growing progressively with years. One of them was a chronic alcohol abuser and reported fast growth of the cervical mass in the past 6 months. The other patient was a compensated diabetic. Two patients were chronic smokers. Apart from that, lab tests and clinical examinations were normal.
The main complaint of the patients was the esthetical deformity, leading to difficulty to move the neck and to use clothes that were too tight. None of them reported dysphonia, dyspnea, stridor or dysphagia.
In the physical examination, they presented multiple symmetrical lipomatosis type I, with lipomas on the neck region (horse collar), deltoid, thoracic and back areas (Figures 1, 2 and 3).
They were submitted to surgical excision of neck lipomatosis, under general anesthesia, through neck incision and careful dissection of diffuse irregular non-encapsulated lipomatous mass. One of the patients was submitted to exeresis of the lipomatous mass on the back of the neck region. Patients progressed well and no recurrences were observed in the six-month follow-up (Figure 4, 5 and 6).
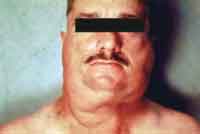

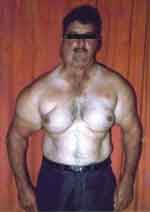
Figures 1, 2, 3. Patients with MSL type I with symmetrical lipomatous accumulation on the neck, dorsum, deltoid and upper thoracic regions.

Figure 4. Early postoperative aspect. Note the significant esthetical improvement.

Figure 5. Irregular non-encapsulated cervical lipomatous mass measuring in its longest axis 12 cm and weighting nearly 900grams.
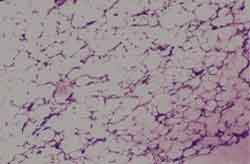
Figure 6. Histology and clinical pathology studies of the lipomatous mass show well-differentiated fatty tissue, compatible with lipoma.
Madelung's disease is characterized essentially by accumulation of diffuse and symmetrical fatty tissues on the cervical region, which can affect the shoulders, dorsum and upper limbs. There are also other areas of the body that may be affected, such as armpit, inguinal region and internal aspect of the thighs. As a rule, the face, feet and hands are not affected5. The clinical progress of the disease is variable. Normally, there is an initial period of quick growth for months or years followed by a long period of stabilization or slow progression of the disease6.
It affects predominantly Caucasian men (15M: 1W), with higher incidence among Mediterranean peoples, being that 1 in each 25,000 Italians develop the disease. The fat deposits are present after the age of 20 years, more commonly between 30 and 60 years. About 60 to 90% of the patients have previous history of moderate to severe alcohol abuse5, 6, 7, 10. Only one of the three patients studied here was a chronic alcohol abuser. It is believed that the effects of lipogenesis, anti-lipolysis and reduction of lipid oxidation of alcohol play an important role in the development of adipocyte hyperplasia in susceptible subjects6.
Izu et al. reported a case of the association between the disease and rhinophyma (benign and progressive hypertrophy of the nose involving connective tissue, sebaceous glands, blood vessels and fatty tissue), a disease that shows close correlation with alcohol abuse1.
Enzi classified MSL in 2 types: type I, in which the fat deposits are circumscribed, forming non-encapsulated masses distributed symmetrically in the upper portion of the body. There are lipomas on the neck region (horse collar), deltoid area (pseudo-athletic appearance) and on the back, giving the false impression that the patient has a vertebral spine kyphosis (humpback)5, 11, 12.
Fat deposits grow slowly throughout the years and the patients look for medical care owing to the esthetical deformity. In advanced cases, there may be compression of the aerodigestive tract, causing dyspnea, stridor and dysphagia, which are more severe complications of the disease5. The lipomatous deposits can infiltrate into the mediastinum and compress the trachea and vena cava, and in some cases, they may also affect the vocal folds and the recurrent laryngeal nerve, leading to dysphonia 5, 11, 12. We can normally observe atrophy of the non-lipomatous fatty tissue, so as that the body mass index (BMI) is reduced5. The three cases reported here were classified as type I MSL.
In type II, the distribution of lipomas is diffuse, and the patient normally seems to be obese. In addition to the upper region of the body, the inguinal and abdominal regions are frequently involved, and there is no affection of the mediastinum or compression of the aerodigestive tract. BMI is normally increased5, 6, 11, 12.
Carlsen et al. suggested the existence of a third variant of the disease, which would represent its congenital form, located predominantly around the trunk6.
According to Enzi, the most frequent sites of lipomas in MSL are: anterior and posterior neck region (100% of the cases), retroauricular (95%), deltoid region (84%), trunk (60%), abdominal region (58%), inguinal region (42%) and lower limb superior portions (42%)9.
There are cases described in the literature of fatty infiltration on the tongue, as reported by Vargas Diez et al., who described a case of Madelung's disease that evolved to symmetrical and gradual increase of the tongue (macroglossia), resulting in swallowing and speech difficulties10.
Laryngeal involvement was primarily described in the French literature - a case of lipomatosis involving ventricular folds and posterior commissure. Moretti and Miller, in 1973, described one case of Madelung's disease associated with moderate edema of the laryngeal mucosa, especially the epiglottis and supraglottis, with swollen ventricular folds of yellowish aspect and significantly reduced laryngeal lumen2.
Other abnormalities and pathological conditions have been associated with Madelung's disease, such as hematological disorders (especially macrocytic anemia), hepatic, endocrine, renal and metabolic disorders, and peripheral neuropathy. It is believed that such conditions are due to abusive alcohol and nicotine use. Similarly, subjacent to Madelung's disease, we can find hypopharynx and tongue carcinomas and bronchogenic carcinomas of metastatic cells or oat cell carcinomas5, 13. Of the three treated patients, two were chronic smokers and one of them was a compensated diabetic patient. Upon clinical examination and lab tests, there were no other associated pathological conditions.
Peripheral neuropathy, owing to the high prevalence and morbidity, is a significant clinical finding in these patients. It may be sensorial, motor or mixed. Autonomic manifestations may be present, affecting preferably the lower limbs. The most common findings include reduction of vibration sensitivity (75%), reduction of muscle force (66%), reduction of osteotendinous reflexes (66%), muscle atrophy (59%) and hypoesthesia (40%). Among the neurovegetative abnormalities, we can include excessive sudoresis, rest tachycardia, gustatory abnormalities, sexual impotence and, if present, they are markers of poor prognosis, sometimes associated with sudden death5, 9.
The diagnosis is normally defined by the clinical history and physical examination. However, there are complementary tests that should be performed to exclude other pathologies such as angiolipoma, neurofibroma, diffuse lipomatosis of the trunk or limbs, and especially liposarcoma 14. The requested imaging exams are computed tomography scan and/or magnetic resonance imaging, being that the most common findings are lipomatosis in characteristic sites, calcification or ossification in the lipomas, deformity or narrowing of the trachea, venous stasis of the thorax wall and absence of abdominal, retroperitoneal and pericardial masses5.
Biopsy is essential to exclude malignancy. There is only one case reported of malignant degeneration of the disease to mixoid liposarcoma 5, 10. Hojaij et al. reported a case of Madelung's disease associated with epidermoid carcinoma of the pyriform sinus, in which the patient, who was an alcohol abuser and smoker for 35 years, presented a neck tumor mass for at least 10 years and dysphonia for 2 months. Upon laryngoscopy, they detected an ulcerative-infiltrative lesion in the right pyriform sinus with ipsilateral vocal fold paresis, confirmed by biopsy as being of grade I, demonstrating the frequent synchronism between Madelung's disease and upper aerodigestive tract tumors8.
The differential diagnosis should include lipomas (mesenchymal neoplasia is more frequent, normally located and in small number), angiolipoma, neurofibroma, hyperbenoma and hyperaldosteronism. It is suspected of the latter is in the initial period of the disease, when only the buffalo humpback is present5, 6. Leffell et al. reemphasized the importance of differentiating MSL from multiple family lipomatosis (MFL). MFL is more common on the third decade of life, involving predominantly the forearms and thighs; it is hereditary, not related to alcohol abuse and even though it affects preferably men (2M:1W), there are family cases described in which all female members of the family were affected15.
Another entity that is part of the differential diagnosis with MSL is decrum painful lipomatosis, characterized by painful manifestation; it preferably affects female patients, especially during menopause13.
Etiopathogenesis of MSL is still obscure. Biochemical analysis and clinical pathology studies revealed, however, some interesting aspects. The proliferation of lipomatous tissue is due both to the differentiation of preexisting adipocytes and to neoplasic cellular replication. This disorder is thought to be associated with a defect of adrenergic lipolysis, a fact attributed to a dysfunction of adipocyte cyclic AMP, making the cells to become autonomous and expanding in an ordered form. The neoadipocytes are smaller than regular adipose cells not involved in the process and are structurally identical to normal brown fat cells5, 8.
Another theory refers to the location of lipomas that correspond to the deposit sites of fetal brown fat8. Persistence and hyperplasia of the tissue after childhood would result in adipose tissue, leading to accumulation of triglycerides in brown adipocytes, leading to hyperplasia 5. It has also been noticed that there is axonal degeneration, related or not to alcohol use and mitochondrial DNA abnormalities, observed in tumor cells, also pointed out as a probable cause of the disease8.
There is one case of MSL described in the literature of a patient who was not an alcohol abuser nor diabetic, with no other systemic abnormalities and no family history of the disease, who had chronic actinic dermatitis and use of high doses of corticosteroids (greater than 40mg/day), showing another possible etiopathogenic component11.
Histologically, the lipomatous tissue cells are not distinguishable from the normal fat cells, despite the fact that ultrastructural studies have shown that adipocytes of MSL are larger and multi-vacuolated. Moreover, there are reports of the existence of fibrous tissue septa that extend from the lipomatous accumulation towards to the adjacent areas, being responsible for the known difficulty to surgically dissect lipomatous masses. Biochemical analysis revealed an elevated concentration of triglycerides in adipocytes of lipomatous deposits when compared to the cells of normal adipose tissue even in patients who have Madelung's disease.
The treatment presents three main modalities: clinical, surgical and liposuction. In clinical treatment, b2-adrenergic agonists (Albuterol) are used to increase lipolysis and reduce fat accumulation, with questionable efficacy. The patient is also instructed to avoid alcohol intake, to lose weight and correct associated endocrine and metabolic abnormalities, and this type of treatment does not revert or interrupt the progression of the disease that is already in place5, 7.
Surgical excision of lipomas is the standard treatment for Madelung's disease, and the absolute indications are the presence of severe cosmetic deformities and signals of compression of aerodigestive tract (dyspnea and/or dysphagia). Liposuction has the advantage of presenting lower peri-operative morbidity than conventional surgery. It is an extremely important issue in these patients, since they are frequently smokers and alcohol abusers, in addition to having associated neuropathies. Liposuction is valid mainly as complementary therapy, that is, after surgical excision of lipomatous deposits, when there is residual accumulation of fat5-7.
The 3 cases in our study were surgically treated through anterior cervical incision on the collar. One of them underwent posterior interscapular incision combined for the resection of the lipomatous mass on the back area. Patients progressed clinically well, with no early or late postoperative complications, with good esthetical results and we did not observe recurrence in a 6-month follow-up period.
Madelung's disease leads to many sequelae, with elevated morbidity. The recurrence of lipomas is common because they are highly infiltrative, being that the definition of size, location and extension of lipomatous accumulations help the definition of prognosis. The presence of peripheral neuropathy results in worse evolution, since it increases morbidity5.
The death normally occurs as a result of alcohol abuse complications, such as portal hypertension and cerebral atrophy, and not directly by complications of the fatty deposits6.
CONCLUSIONMadelung's disease is a relatively rare condition. Its main characteristics are asymmetry, location of lesions and natural diffusion of fatty deposits, making it a distinct clinical entity. It is more frequent in Caucasian men descendents of Italians and middle-aged. The histology pattern is benign. The etiology is still open ended but the association with alcohol has been clearly defined.
The main problems caused by the disease are esthetical, following the reduction of neck movement. There may be complications resulting from the compression of the aerodigestive tract (dyspnea, stridor and dysphagia) and still, but less frequently, signs and symptoms of upper vena cava compression and dysphonia by the involvement of the recurrent laryngeal nerve. The diagnosis is manly clinical. The imaging exams are important for its prognostic value to determine the topography and extension of lesions, owing to the high incidence of recurrence.
Surgical excision was the treatment of choice in our service for the 3 cases, showing effective and good esthetical outcomes. Liposuction can be used as a complementary treatment and for surgically contraindicated cases. The clinical treatment is not effective and alcohol abstinence does not cause spontaneous regression of lipomas.
Finally, since the risk of malignant transformation is low, clinical follow-up is enough when there is no evidence of infiltration of lipomatous tissue, dispensing imaging follow-up.
REFERENCES 1. Izu R, Gardeazabal J, Béjar J et al. Acase of elephant man phenotype with giant rhinophyma and benign symmetric lipomatosis. Clinical and Experimental Dermatology 1994;19:531-533.
2. Moretti J, Miller D. Laryngeal Involviment in Benign Symmetric Lipomatosis. Arch Otolaryngol June 1973;97:495-496.
3. Boozan J, Maves M, Schuller D. Surgical Management of Massive Benign Symmetric Lipomatosis. Laryngoscope January 1992;102:94-99.
4. Gabriel Y, Chew D, Wedderburn R. Multiple symmetrical lipomatosis (Madelung's disease). Surgery 2001;117-118.
5. Oliveira B, Ramos G, Tomasich F et al. Lipomatose Simétrica Múltipla (Síndrome de Madelung): Relato de caso e revisão da literatura. Revista Brasileira de Cirurgia de Cabeça e Pescoço jan/ago. 1999;23(1-2):29-36.
6. Parmar S, Blackburn C. Madelung's Disease: an uncommon disorder of unknown aetiology? British Journal of Oral and Maxillofacial Surgery 1996;34:467-470.
7. Adamo C, Vescio G, Battaglia M. et al. Madelung's Disease: Case report and discussion of treatmente options. Ann Plast Surg 2001;46:43-45.
8. Hojaij F, Cernea C, Nishio S, Vanderlei F. Doença de Madelung associada a Carcinoma Epidermóide do seio piriforme: relato de caso. Revista Brasileira de Cirurgia de Cabeça e Pescoço jan./ago. 1999;23(1-2):37-38.
9. Araújo L, Rêgo V, Dias N et al. Lipomatose simétrica benigna (Doença de Madelung): relato de caso. Rio de Janeiro: An bras Dermatol nov/dez. 1996;71 (6):495-498.
10. Vargas-Díez E, Daudén E, Jones-Caballero M and García-Diez A. Madelung's disease involving the tongue. J Am Acad Dermatol 2000;42 (3):511-513.
11. Khanna N, Dogra D, Rathi S, Ravindraprasad J. Multiple Symmetrical Lipomatosis in a Patient on Long-term Corticosteroid Therapy. Acta Derm Venereol December, 1995 (Stockh) 76:245-246.
12. Nielsen S, Levine J, Clay R, Jensen M. Adipose Tissue Metabolism in Benign Symmetric Lipomatosis. J Clinical Endocrinol ans Metabolism March 2001;86 (6) :2717-2720.
13. Dusková M, Topinka H. Lipomatosis Benigna Symmetrica - Syndrom Launois-Bensaude (Case report). Acta Chirurgiae Plasicae 1994;36(2):61-63.
14. Uhlin S. Benign Symmetric Lipomatosis. Arch Dermatol Jan 1979; (115):94-95.
15. Leffell D, Braverman M. Familial multiple lipomatosis: report a case and review of the literature. J Am Acad Dermatol 1986;15:275-279.
1 Director, Núcleo de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço de São Paulo.
2 Assistant Physician, Núcleo de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço de São Paulo.
3 Resident Physician, Núcleo de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço de São Paulo.
Study conducted at Núcleo de Otorrinolaringologia e Cirurgia de Cabeça e Pescoço de São Paulo.
Address correspondence to: José Antonio Pinto - Alameda dos Nhambiquaras, 159 Moema 04090-010 São Paulo SP - Tel/Fax (55 11) 5573-1970 - E-mail: japorl@cepa.com.br
Article submitted on April 10, 2002. Article accepted on July 04, 2002.


