INTRODUCTIONParathyroid cysts are rare lesions normally located in the neck and exceptionally in the mediastinum, in about 10% of the cases 1. They are normally asymptomatic and frequently omitted in differential diagnosis of neck masses.
Cysts may be classified as functioning and nonfunctioning depending on the association with primary hyperparathyroidism; most of the cases are nonfunctioning.
Its importance lies in the diagnostic difficulty: it is normally mistaken by thyroid pathology, meaning that it is normally diagnosed only in the surgical act. It is still possible to cause compressive symptomatology, hyperparathyroidism, in addition to recurrent laryngeal nerve paralysis.
The purpose of the present study was to report a case of parathyroid cyst that simulated thyroid nodule, discussing diagnostic aspects.
CASE REPORTMale 49-year-old patient, coming from Sao Paulo, came to the ambulatory of Head and Neck Surgery, Service of Otorhinolaryngology, Hospital Servidor Público Estadual de São Paulo, complaining of neck nodule located in the thyroid gland for about 6 months. He did not report dyspnea, odynophagia, dysphagia or dysphonia. Two years before he had been diagnosed with primary hypothyroidism, taking thyroid hormones on a daily basis. ENT examination did not reveal abnormalities but there was nodular lesion on the neck, specifically located on the right thyroid lobe, of cystic consistency, measuring about 6 x 4cm, non-painful and moving with swallowing.
TSH and T4 free levels were normal and anti-thyroid antibodies were negative, serum calcium corresponded to 10.16 (normal up to 10.2mg/dl) and ionic calcium was 1.18 (normal up to 1.32mmol).
Chest radiological exam evidenced mild deviation of the trachea to the left. Ultrasound (US) defined volumous cyst on the right thyroid lobe measuring approximately 5.6 x 5.4cm, medially displacing thyroid tissue (Figure 1). Computed tomography (CT scan) of the neck showed increase of thyroid gland caused by right thyroid lobe and isthmus affection owing to cystic hypoattenuating image of regular borders without extension into the mediastinum (Figure 2). We conducted fine needle aspiration biopsy of the cystic lesion, whose cytological analysis revealed acellular smears comprising protein amorphous material, cyanophilic, and it was not possible to define the origin of the lesion. The hypothesis of atoxic uninodular goiter indicated right lobectomy and isthmectomy.
The patient was submitted to surgery and, intraoperatively, the staff detected a large cystic lesion measuring 8 x 6cm, with thin walls with aqueous content on the right thyroid lobe (Figure 3), including cleavage plan between it and the right thyroid lobe. We identified the right upper parathyroid and recurrent laryngeal nerve on the same side. The clinical pathology result confirmed the diagnosis of parathyroid cyst. Fine needle aspiration biopsy of the cyst with aspiration of 10ml water-clear fluid (Figure 4). The parathyroid hormone dosage of liquid was > 2500 pg/ml.
The patient progressed without complications after the surgery and dosages of serum and ionic calcium were 8.5mg/dl and 1.23mmol, respectively.
DISCUSSIONParathyroid cysts are pathologies considered to be rare, comprising about 250 cases described in the literature 1,2,3. The exact incidence is still discussed, given that in one study its occurrence ranged from 0.08 to 3.4% of the cases of thyroid or parathyroid resection 4. In a study with thyroid and parathyroid specimens examined within a period of 15 years, parathyroid cysts were found in 0.6% 3. Analyses in autopsies revealed 40 to 50% of parathyroid glands that contained asymptomatic microcysts 5, given that in only 1 to 3% they presented as a neck mass 6.
Parathyroid cysts occur in both genders, with the proportion of 2.5:1 women to men, normally at the 4th and 5th decades of life 7. The vast majority is located in lower parathyroid glands, described from the mandible angle to the mediastinum, with slight predominance on the left 5. Similarly to other parathyroid lesions, cysts may occur in ectopic locations, especially the thymus and mediastinum. About 10% of the cases are visualized in the mediastinum, normally in the anterior region 1.
Pathogenesis of parathyroid cyst is uncertain, and there are some theories that explain its origin: (1) as embryological remains of 3rd and 4th branchial arches, causing increase in volume by accumulation of secretion forming a macrocyst; (2) degeneration, infarction or hemorrhage of parathyroid or gland adenoma; (3) coalescence of microcysts of normal or adenomatous parathyroid aspect; (4) persistence of Kustneiner canal, which are vesicular canals in fetus or gland remains, and (5) retention of parathyroid hormone (PTH) in colloid vesicles 8. Despite these embryological theories, there are no reports of parathyroid cysts in children 1,3,8,9.
Parathyroid cysts may be classified as functioning and nonfunctioning depending on the association with hyperparathyroidism. The functioning type normally results from degeneration of true parathyroid adenoma 9; however, Calandra et al. 8 found many different simple cysts associated with hyperparathyroidism. In most cases reported in the literature, less than 10% are functioning; differently from Calandra et al.8 in which 10 out of 11 patients with parathyroid cysts had parathyroidism, evidencing hypercalcemia, hypophosphatemia and increase of serum PTH. Patients with functioning cysts tend to be men, being 1.6 times more frequent than in women and of older age 1, 3. Nonfunctioning cysts are described as the most common, predominantly in women. They are normally described as asymptomatic neck masses. According to Clark et al.1, in both types, the content of the cyst presents high concentrations of PTH1,3,9.
Most parathyroid cysts are asymptomatic. The main symptoms caused by the local compressive effect of the lesion when it becomes larger include dysphagia, hoarseness, pain, neck mass or dyspnea by tracheal deviation 5. Hoarseness is caused by vocal fold paresis, which can be explained by edema and fibrosis of recurrent laryngeal nerve combined with pressure or traction of the cyst wall 10. There are also symptoms resulting from hyperparathyroidism, with elevation of serum calcium and repercussions at the central nervous and neuromuscular systems, gastrointestinal tract, kidneys and cardiovascular system 5. The common presentation of parathyroid cyst is, however, asymptomatic neck mass, as observed in our case. They are frequently mistaken by thyroid pathology, as described by Piccinato et al.2 or cysts of other nature. They may also be occasionally found during surgical exploration or radiological imaging tests 3. The physical examination shows solitary mass of cystic consistency, non-painful and mobile during swallowing 5,8. Other characteristic is that parathyroid cysts may vary concerning size, as demonstrated by Coates et al.11, adding more difficulty to diagnosis.
Differential diagnosis extends from thyroglossus duct cyst, branchial arch cyst, thyroid adenoma to parathyroid carcinoma 6, 11. Preoperative suspicion of parathyroid cyst is extremely important, considering the complexity of the diagnostic confirmation, especially because most of them are diagnosed intraoperatively or in the clinical analysis of the surgical specimen.
Among the complementary tests that can be helpful, fine needle aspiration biopsy is well defined as first line exam in investigation of neck masses owing to its technical facility, low cost and minimum invasion of tissues. In some cases, it may prevent unnecessary surgery or it may support surgical planning, providing analysis of characteristics of the cyst's content and cytological aspects 12. Absher et al.12 studied 12 cases of parathyroid cysts and their main findings were water-clear liquid, aqueous and slightly bloody, predominantly acellular, with rare inflammatory cells or macrophages. This study showed difficulty to differentiate parathyroid cyst from some thyroid lesions, such as follicular lesions, which may exist concomitantly with these pathologies 9,12.
Most studies agree that the presence of fluid, glossy, aqueous liquid is highly suggestive of parathyroid cyst, indicating verification of PTH dosage in the liquid to determine the diagnosis 5,7,12. The analysis of intra-cyst liquid containing high levels of PTH portion C-terminal alone or combination of PTH portion N-terminal with high serum level is diagnosed as parathyroid cyst 5. Both in functioning and nonfunctioning cysts, dosage of intra-cyst PTH is higher than serum levels. In nonfunctioning cysts the level of PTH reported is 6 - 416 pg/ml, with normal serum levels, whereas in functioning cysts there are higher levels of 2000 - 6000pg/ml10. In our case, the value of PTH in the cyst liquid was >2500 pg/ml, differently from the literature given that it was a nonfunctioning cyst.
Image exams are indicative of cystic neck solitary lesion, but they are not conclusive 5. Ultrasound (US) showed a cystic, anechoic structure with thin walls and posterior hyperechoic enhancement 3, 13. According to Gooding et al.8 parathyroid cysts may not be differentiated from thyroid cysts through ultrasound. CT scan and Magnetic Resonance Imaging (MRI) demonstrate only neck mass with cystic content and their anatomical relations. Thyroid scintigraphy may reveal the presence of nonfunctioning cysts, but it does not distinguish the lesion in thyroid or parathyroid 1,3.
Histology characteristics of parathyroid cysts are normally thin internal walls, comprising connective tissue and parathyroid cell islands, a solitary layer of cuboid and columnar cells with glycogen positive staining 5, 7. The presence of parathyroid tissue on the cyst wall is diagnostic indication. The cyst may be adhered to the thyroid tissue, but it is easily separated from it 1, 5.
Treatment for nonfunctioning cysts without complications may be US-guided aspiration, once there are no reports of malignancy 14. Sclerotherapic substances may be introduced even though they are not universally accepted owing to complications, such as neurotoxicity or recurrent laryngeal nerve paralysis. Okamura et al.15 in their study with 5 patients, out of which 4 were treated with sclerotherapic agents, suggested that tetracycline has low risk, low cost and is effective in treating parathyroid cysts. In case of recurrence of cysts complicated by symptoms of dysphagia, dyspnea or recurrent laryngeal paralysis, primary treatment should be surgical. The treatment of functioning cyst is always surgical 15. These lesions with hormonal alterations have high risk of affecting other parathyroid glands, which can be identified in the surgical act 1. Macroscopic observation of parathyroid cysts intraoperatively is of a solitary unilocular cyst adhered to the thyroid tissue, but the defined cleavage plan has thin, glossy and clear-content walls, in the lower portion of the neck. Mediastinum cysts are normally treated with surgery 14. In many series, including the one by Rosenbrg et al.3, lobectomy or partial thyroidectomy were advocated in treating parathyroid cysts. Preoperative consideration, however, about the diagnostic possibilities, intraoperative frozen analysis and fluid exam may prevent excision of thyroid gland.
This case report exemplifies diagnostic difficulties in preoperative parathyroid cysts, confirming the literature data and drawing attention to the importance of including it in the differential diagnosis of neck cysts.
REFERENCES1. Clark OH. Parathyroid cysts. Am J Surg 1978; 135: 395-402.
2. Piccinato CE, Cherri J, Llorach-Velludo MAS, Iazigi N, Alves MAD. Cisto não funcionante de paratireóide simulando nódulo tiróideo. Rev Paul Med 1990; 108: 236-238.
3. Rosenberg J, Orlando R, Ludwig M, Pyrtek LJ. Parathyroid cysts. Am J Surg 1982; 143: 473-480.
4. Mallete LE. The functional and Pathologic spectrum of parathyroid abnormalities in hyperparathyroidism. In: Bilezikian JP, Levine M, Marcus R, eds. The parathyroids. New York, NY: Raven Press; 1994: 423-455.
5. Fortson JK, Patel VG, Henderson VJ. Parathyroid cysts: a case report and review of the literature. Laryngoscope 2001; 111: 1726-1728.
6. Alvi A, Myssiorek D, Wasserman P. Parathyroid cyst: current diagnostic and management principles. Head Neck 1996; 18: 370-373.
7. Ihm PS, Dray T, Sofferman RA, Nathan M, Hardin NJ. Parathyroid cysts: diagnosis and management. Laryngoscope 2001; 111: 1576-1578.
8. Calandra DB, Shah KH, Prinz RA, Sullivan H, Hofmann C, Oslapas R, Ernst K, Lawrence AM, Paloyan E. Parathyroid cysts: a report of eleven cases including two associated with hyperparathyroid crisis. Surgery 1983; 94: 887-892.
9. Petri N, Holten I. Parathyroid cyst: report of case in mediastinum. J Laryngol Otol 1990; 104: 56-57.
10. Shields TW, Immerman SC. Mediastinal parathyroid cysts revisited. Ann thorac Surg 1999; 67: 581-590.
11. Coates G, Pearman K, Holl-Allen RT. Recurrent nerve palsy due to parathyroid cyst. Int Surg 1991; 76: 192-193.
12. Absher KJ, Truong LD, Khurana KK, Ramzy I. Parathyroid cytology: avoiding diagnostic pitfalls. Head Neck 2002; 24: 157-164.
13. Gooding GAW, Duh QY. Primary Hyperparathyroidism: functioning hemorrhagic parathyroid cyst. J Clin Ultrasound 1997; 25: 82-84.
14. Sen P, Flower N, Papesch M, Davis A, Spedding AV, Path MRC. A benign parathyroid cyst presenting with hoarse voice. J Laryngol Otol 2000; 114: 147-148.
15. Okamura K, Ikenoue H, Sato K, Yoshinari M, Nakagawa M, Kuroda T, Fujishima M. Sclerotherapy for benign parathyroid cysts. Am J Surg 1992; 163: 344-345.
 Figure 1.
Figure 1. Neck ultrasound evidenced volumous cyst on the right thyroid lobe measuring 5.6 x 5.4cm, medially displacing the thyroid tissue.
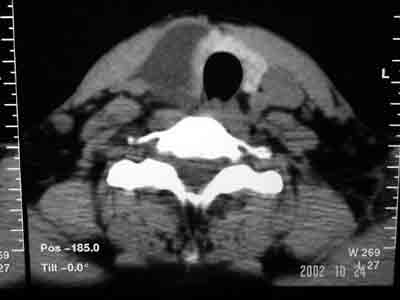 Figure 2.
Figure 2. CT scan of the neck showing increase of thyroid gland because of right thyroid lobe and isthmus, showing hypoattenuating cystic image of regular borders without extension into the mediastinum.
 Figure 3.
Figure 3. Intraoperative aspect demonstrating large cystic lesion measuring 8 x 6cm with thin, glossy walls of aqueous content adhered to right thyroid lobe.
 Figure 4.
Figure 4. We conducted fine needle aspiration biopsy of the cyst intraoperatively with aspiration of 10ml of water-clear fluid.
1. Resident Physician, Service of Otorhinolaryngology and Head and Neck Surgery, Hospital do Servidor Público do Estado de São Paulo
2. Head of the Division of Head and Neck Surgery, Hospital do Servidor Público Estadual de São Paulo
3. Assistant Physician, Service of Endocrinology, Hospital do Servidor Público Estadual de São Paulo
Affiliation: Hospital do Servidor Público do Estado de São Paulo
Address correspondence to: Danielle Andrade da Silva
Av. Jurema nº 80 apt 15 - Moema / São Paulo - SP CEP 04079-000
Tel: 55 11 5052-3093 - Cel: 55 11 8132-9620
Email: andradeds@hotmail.com
Study presented at 33ª Jornada Paulista de Radiologia, in May 2003, in Sao Paulo, and at XIX Congresso Brasileiro de Cirurgia de Cabeça e Pescoço, in September 2003.


