INTRODUCTIONFungal sinusitis is divided, for simplification reasons, into 2 main groups, namely: (1) invasive form, which is subdivided into acute and chronic; (2) noninvasive form, which is divided into fungal ball (mycetoma) and allergic fungal sinusitis. The histological analysis of involved tissues, such as presence or absence of vascular invasion, is the basis for differentiation between invasive and noninvasive forms. The development of different forms of fungal sinusitis depends entirely on the immune status of the patient, and acute or chronic invasive form occurs normally in immunodepressed patients, fungal ball and allergic fungal sinusitis in atopic patients. The classification is, therefore, based on host immune response in view of fungi 2.
In chronic invasive form, also called indolent, the duration of disease evolution is greater than four weeks, differently from the acute invasive form, whose evolution lasts less than 4 weeks 3. Moreover, as previously referred, the host is normally immunocompetent, and Aspergillus is the most common pathogen. In Computed tomography scan (CT scan) we can observed uni or bilateral paranasal sinuses velamentum, with hyperattenuation foci, suggestive of fungal colonization 4. The treatment is based on surgical debridement and antifungal agents are necessary if there is intracranial or orbital invasion 1.
Mycetoma or fungal ball is characterized by unilateral impairment of paranasal sinuses most of the times by Aspergillus, maxillary sinus is the most frequently affected sinus, followed by sphenoid. Symptomatology imitates bacterial sinusitis, but the patient may be asymptomatic 5. In paranasal sinuses CT scan, we can observe unilateral velamentum of paranasal sinuses with hyperattenuation foci, which represents calcifications and hyphae 5. It is installed in immunocompetent hosts, normally solved with surgical debridement and sinusal aeration, rarely followed by recurrence 1.
Allergic fungal sinusitis, in turn, is the most common form of sinusal fungal infection 6. It is a chronic form that develops in atopic subjects, with symptoms similar to bacterial chronic sinusitis, many times with history of nasal polyposis 6. Bent and Kuhn7 developed the following criterion for allergic fungal sinusitis: (1) type I hypersensitivity; (2) nasal polyps; (3) characteristic CT scan findings, with hyperattenuation foci owing to allergic mucin and bone destruction present in 30-50% of the cases 1; (4) positive fungal culture; (5) allergic mucin with fungi and without signal of tissue invasion. Allergic mucin is characterized by eosinophils, Charcot-Leyden crystals and hyphae6. The most frequently fungi involved in this type of fungal sinusitis are Bipolaris, Curvularia and Alternaria3. Treatment includes surgical debridement and use of antifungal agents is reserved for cases of tissue invasion 1.
Acute invasive fungal sinusitis affects, most of the time, immunodepressed subjects, whose main etiologic agents are fungi Mucor and Aspergillus, among others1. The term mucormycosis is used to refer to all fungal infections caused by fungi from class Zygomycetes and order Mucorales, whose most common representative is Rhizopus oryzae, responsible for 60% of all forms of mucormycosis, in addition to Mucor, and Absidia3.
Any type of immunodeficiency can take to the onset of mucormycosis, but diabetic ketoacidosis is the most frequent triggering factor 3. Even though it is more common in immunodeficient patients, mucormycosis may affect healthy subjects, such as reported by Santana et al.8.
Mucormycosis may be manifested in different clinical forms, such as pulmonary, gastrointestinal, central nervous system, cutaneous and systemic forms, but the most common is still the rhinocerebral presentation 9.
Yohia et al.10 reviewed 208 cases of rhinocerebral mucormycosis between 1970 and 1993 and found as the main symptoms: fever (44%), nasal ulcer or necrosis (38%), periorbital or facial edema (34%), reduction of visual acuity (30%), ophthalmoplegia (29%), sinusitis (26%) and headache (25%). In fact, such as in any immunodepressed patient, especially those with diabetic ketoacidosis, with symptoms of rhinosinusitis without improvement after conventional antibiotic treatment, we should bear in mind the diagnosis of mucormycosis.
The histological diagnosis of mucormycosis is based on the finding of non-septated hyphae or few septa, contrarily, for example, of Aspergillus, whose hyphae is very narrow and frequently septated at 45o angles 5.
Paranasal sinuses CT scan may show tissue invasion and necrosis, bone erosion and cavernous sinus thrombosis. Magnetic resonance imaging (MRI) with or without gadolinium, is the best method to assess early affections to vessels such as carotid artery and cavernous sinus thrombosis. MRI is also the best form to study possible intracranial extension 11.
The main objective of surgical debridement is to remove maximum devitalized tissue in addition to defining the appropriate sinusal drainage 12. In recent years, endoscopic surgery to surgically treat mucormycosis has gained more attention 13. In the study by Jiang et al.14, six patients with mucormycosis were treated with amphotericin B and endoscopic surgery and only one of them died of internal carotid artery obstruction.
The administration of amphotericin B increases survival from 37 to 79% in diabetic patients and from zero to 47% in non-diabetic patients 15. For effective control of the disease, we should administer it in high doses that range from 0.8 to 1.5 mg/kg/d16, and in high dosage it is considered nephrotoxic. The association of amphotericin B with cholesterol sulfate, also called amphotericin B with colloid dispersion or liposomal, is a formulation capable of releasing high doses of drug with reduced nephrotoxicity owing to abnormalities in pharmacological distribution, and it is a treatment option of mucormycosis in patients that do not respond to conventional treatment. Tkatch et al. 15 reported a case of mucormycosis in diabetic patients in which liposomal amphotericin B was used with good case progression. Some studies showed that efficacy is the same between the use of liposomal amphotericin B and traditional amphotericin B 17,18. Rios-Gonçalves et al.19 reported survival of 2 cases treated with amphotericin B followed by surgical treatment. Other authors recommended liposomal amphotericin B since it causes less toxicity allowing use of higher dosage, with better responses to treatment 20.
Another alternative is the use of liposomal nystatin, as reported by Mileshkin et al.21 in a patient with mucormycosis refractory to treatment with liposomal amphotericin B; the patient had good tolerance and no evidence of nephrotoxicity, with evident clinical improvement.
The adjuvant use of hyperbaric chamber has been employed in a small number of cases, with good results. Hyperbaric oxygen increases tension of oxygen in sick tissues, which some in vitro studies suggested having fungostatic action 22.
CASE REPORTA.M.B., 51-year-old female patient , born in Piratininga - SP, with history of diabetes mellitus for 10 years, using insulin NPH 40U in the morning and 30U in the afternoon, presented diabetic decompensation - hyperosmolar comma - and she was hospitalized in the intensive care unit with severe abdominal pain. On the second hospitalization day, she reported significant left ocular pain, periorbital edema, proptosis, fever and fetid discharge from the fistulous path on the left internal eye canthus (Figure 1), which progressed to amaurosis on the left. Paranasal sinuses CT scan was performed at axial and coronal sections, which identified significant increase of soft parts together with the left orbit including some gas points, associated with highlighted area in capsular region of the frontal lobe, which could represent cerebritis (Figures 2 and 3). In view of the decompensation of the underlying disease and quick progression of the orbital abscess, the Ophthalmology team conducted orbital drainage. Owing to the persistence of the case, she was surgically approached two months later together by the team of Otorhinolaryngology and we used transmaxillary sinusectomy on the left during which we visualized thick white secretion on the ethmoid region. In the clinical pathology analysis, the findings were mucosa recovered by respiratory epithelium with inflammatory process and the septated hyphae led to final diagnosis of zygomycosis. We conducted paranasal sinuses CT scan after the surgical procedure and it revealed maintenance of naso-cutaneous fistula and attenuation material of soft parts together with the orbit apex and inside the left maxillary sinus (Figures 4 and 5). Even though there was persistence of naso-cutaneous fistula, she presented progressive improvement by using amphotericin B (total dose of 1,015 mg) and after one month of treatment, the patient no longer had discharge from the fistula. She was referred to the Plastic Surgery Center and after being completely asymptomatic for one year, she was submitted to cosmetic surgery on the left naso-orbital region, and currently the patient is very satisfied with the surgical outcome (Figure 6).
DISCUSSIONMucormycosis normally affects immunodepressed patients, such as diabetic patients with ketoacidosis. The fungus in general starts its invasion through the nasal mucosa, with affection of paranasal sinuses, followed by hard palate, orbit and brain erosion 17. It is in the opposite spectrum of allergic fungal sinusitis, which is the most common form of sinusal fungal infection, which affects hypercompetent subjects - atopic subjects 6.
The progression of the disease leads to a sequence of symptoms that starts with sudden facial pain or unilateral orbital pain, many times with nasal obstruction and necrotic nasal secretion. There may be dark lithic lesion of the nasal mucosa or nasal dorsum, orbital and facial cellulitis, fever, palpebral ptosis, amaurosis, ophthalmoplegia, corneal anesthesia, leading to coma and death 10.
The sequence of symptoms may vary depending on where the fungal invasion started and its progression is subject to the immune state of the patient. Depending on the impaired structures, the disease is described under different names. For example, cerebral mucormycosis, craniofacial mucormycosis, rhinocerebral mucormycosis, rhinocerebral zygomycosis, etc.
Our patient presented nasal fossa impairment, plus paranasal sinuses, orbit, periorbit and small cerebral invasion, close to the anterior fossa. If the carotid artery is affected, the prognosis is normally more obscure 11. Galetta et al.11 described two cases of rhinocerebral mucormycosis with internal carotid artery thrombosis who survived. The definition of orbital involvement includes visual affections, dextraorbital muscle deficit, ophthalmoplegia, proptosis or periorbital cellulitis 9. CT scan is the most appropriate imaging test for diagnosis and follow-up of progression of patients with suspicion of fungal sinusitis 4, and in these patients the exam is essential to define extension of the lesion.
The first stage of treatment of invasive fungal sinusitis is the compensation of the underlying disease 3, which in the case of the patient in our report, it was normalization of glucose levels.
Early diagnosis and surgical approach are the most important points associated with good progression of mucormycosis treatment 15. Submitted to transmaxillary sinusectomy, we observed much necrotic material, and the clinical pathology confirmed clinical impression of zygomycosis. We did not manage to identify the agent of tissue invasion in the material. In postoperative assessment, we were not sure about exenteration of left orbit, since there were signals of resistant infection, but the literature has shown that there is no difference in the progression of patients with preservation or not of the orbit, so it was preserved 1. The introduction of amphotericin B, together with antibiotic therapy which had already been used, brought improvement of the clinical picture of the patient, and it remained only a nasocutaneous fistula, with no other symptoms.
The introduction of amphotericin, according to some authors, has favored survival of patients with mucormycosis. Rios-Gonçalves et al.19, in 1991, followed two diabetic patients with similar clinical pictures to the one our patient presented, followed the same management and succeeded. Similarly, Santana et al.8 reported a case of paranasal sinuses and orbital mucormycosis with good results. According to Mileshkin et al., an alternative is liposomal amphotericin with less toxicity, allowing the use of higher doses21. Leenders et al.20 conducted a randomized multicenter study comparing efficacy of liposomal amphotericin B and non-liposomal amphotericin B and found better results in the patients treated with the first option.
The endoscopic approach may also be used, but preoperatively it is necessary to use CT scan to identify exactly the extension of the infectious process, given that depending on the extension, if complete endoscopic removal 14 is not possible, it is preferable to conduct the surgery with open approach for complete debridement. Thus, in advanced cases in which there is impairment of pterygomaxillary fissure or involvement of the orbit, inferior orbital fissure, temporal and infratemporal fossa, buccal space, open traditional surgical debridement should be performed 9. Given that there are no studies confirming that orbital exenteration increases survival, the eye should be only removed when there are signals of retina artery thrombosis, necrosis of orbital apex or orbital invasion 1. Qingli et al.12, however, reported one case of rhinocerebral mucormycosis with retina artery and posterior nasal ciliary artery necrosis in which they did not perform exenteration of orbit, but the final clinical result was good. Thus, in the case of the patient reported here, we decided for open access but without orbit exenteration.
CONCLUSIONSurvival of our patient resulted from some combined actions that started with immediate control of the decompensated underlying disease, eliminating the hyperosmolar coma, comprehensive surgical debridement and use of amphotericin B, together with mild cerebral impairment - they were key factors for the success of management.
Mucormycosis should be considered a severe and potentially fatal disease and for this reason it is necessary to have high suspicion levels in view of acute sinusal symptoms in immunodepressed patients, including mucormycosis among the key differential diagnoses.
REFERENCES1. Blitzer A, Lawson W. Fungal infections of the nose and paranasal sinuses. Otolaryngol Clin North Am 1993; 26 (6): 1007-35.
2. Ence BK, Gourley DS, Jorgensen NL. Allergic fungal sinusitis. Am J Rhinol 1990; 4: 169-78.
3. Ferguson BJ. Definitions of fungal rhinosinusitis. Otolaryngol Clin North Am 2000; 33(2): 227-35.
4. Stringer SP, Ryan MW. Chronic invasive fungal rhinosinusitis. Otolaryngol Clin North Am 2000; 33 (2): 375-87.
5. Ferguson BJ. Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am 2000; 33 (2): 389-98.
6. Houser SM, Corey JP. Allergic fungal rhinosinusitis pathophysiology epidemiology and diagnosis. Otolaryngol Clin North Am 2000; 33 (2): 399-409.
7. Bent JP, Kuhn FA. Antifungal activity against allergic fungal sinusitis organisms Laryngoscope 1996; 106: 1331-4.
8. Santana NOR, Pinheiro GB, Kehrle HM, Faria IP, Estrella CN. Mucormicose de seios paranasais e órbitas em paciente imunocompetente: relato de caso e revisão da literatura. Rev Bra Otorrinolaringol 2001; 65(5) 727-30.
9. Alobid I, Bernal M, Calvo C, Vilaseca I, Berenguer J, Alós L. Treatment of rhinocerebral mucormycosis by combination of endoscopic sinus debridement and amphotericin B. Am J Rhinol 2001; 15: 327-31.
10. Yohia RA, Bullock JD, Aziz AA, Market RJ. Survival factors in rhinoorbital cerebral mucormycosis. Surv Ophthalmol 1994; 39: 3-22.
11. Galetta SL, Wulc AE, Goldberg HI, Nichols CW, Glaser JS. Rhinocerebral mucormycosis: management and survival after carotid occlusion. Ann Neurol 1990; 28:103.
12. Qingli L, Orcutt JC, Seifter LS. Orbital mucormycosis with retinal and ciliary artery occlusions. Br J Ophthalmol 1989; 73:680-3.
13. Blokmanis A. Endoscopic diagnosis treatment and follow-up of tumors of the nose and sinuses. J Otolaryngol 1994; 23: 366-9.
14. Jiang RS, Hsu CY. Endoscopic sinus surgery for rhinocerebral mucormycosis. Am J Rhinol 1999; 13: 105-9.
15. Tkatch LS, Kusne S, Eibling D. Successful treatment of zygomycosis of the paranasal sinuses with surgical debridement and amphotericin B colloidal dispersion. Am J Otolaryngol1993; 14 (4): 249-53.
16. Sugar AM. Mucormycosis. Clin Infect Dis 1992; 14: S 126-9 (suppl 1).
17. Strasser MD, Kennedy RJ, Adam RD. Rhinocerebral mucormycosis therapy with amphotericin B lipid complex. Arch Intern Med 1961; 56: 337-9.
18. Fisher EW, Toma A, Fisher PH et al. Rhinocerebral mucormycosis: use of liposomal amphotericin B. J Laryngol Otol 1991; 105: 575-7.
19. Rios-Gonçalves AJ, Rozenbaun R, Salles F, Laun IC, Mendes TP Medeiros P, Vieira ARM, Ramos DD, Chicralla C, Souza MOP, Londero AT. Mucormicose (Zigomicose) rinocerebral. Apresentação de dois casos com sobrevida. Arq Bras Med 1991; 65(3) 287-90.
20. Leenders AC, Daenen S, Jansen RL et al. Liposomal amphotericin B compared with amphotericin B deoxycholate in the treatment of documented and suspected neutropenia- associated invasive fungal infections. Br J Haematol 1998; 103: 205-12.
21. Mileshkin L, Slavin M, Seymour JF, McKenzie A. Successful treatment of rhinocerebral zygomycosis using liposomal nystatin. Leukemia and Lymphoma 2001; 42(5): 1119-23.
22. Couch L, Theilen F, Mader JT. Rhinocerebral mucormycosis with cerebral extension successfully treated with adjunctive hyperbaric oxygen. Arch Otolaryngol 1988; 114: 791-4.
 Figure 1.
Figure 1. Skin retraction with nasocutaneous fistula close to the left internal orbit canthus.
 Figure 2.
Figure 2. Axial section showing significant facial asymmetry with increase of soft parts on the left orbit with some gas points present.
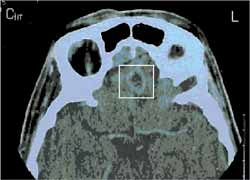 Figure 3.
Figure 3. Axial section evidencing area of capsular highlight in the frontal lobe (cerebritis).
 Figure 4.
Figure 4. CT scan paranasal sinuses - axial section. Postoperative image showing nasal-cutaneous fistula and presence of soft tissue material close to the orbit apex.
 Figure 5.
Figure 5. Paranasal sinuses CT scan - coronal section. Postoperative image showing presence of soft part material inside the left maxillary sinus.
 Figure 6.
Figure 6. Patient after the closure of nasocutaneous fistula.


