IntroductionParangangliomas are tumors of the neural crest arising from paraganglionic tissue, in the paravertebral region, and are associated with cervical vessels, cranial nerves and the autonomic nervous system. Paraganglionic cells can produce and store vessel-active substances and neurotransmitters, such as catecholamine, epinephrine and norepinephrine, as well as a variety of hormones, including serotonin, gastrin and somatostatin 1.
Carotid body tumors account for 60-70% of the head and neck paraganglionic lesions, whose top incidence occurs between the ages of 45 and 50 years1,2,3. There are nearly 600 cases reported in literature4. Presence of bilateral lesion is observed in only 2-10% of the cases3.
The authors presented one case of bilateral carotid body paraganglioma, as well as its diagnostic features and treatment.
A Case StudyMCS, a 42-year-old Caucasian female from Sao Paulo, arrived at our service complaining of a 5-year progressively growing neck tumor. The patient stated that for the past 3 years, she felt mild local pain, but with no other associated symptoms. Local regional examination did not reveal any lesions on the aerodigestive tract upper airways. Clinically, a 5.0x3.0 cm nodular lesion was found in the upper right jugular-carotid region. It was a hard-consistency pulsatile painless lump with slightly regular surface, vertically fixed, horizontally mobile, found on the right II and III levels. On the left side, a 2.0 x 1.0 cm lump - with the same characteristics - was occupying level II. No palpable lymph nodes were observed. Nasopharyngoscopy was normal.
Needle aspiration of the lesion had been previously performed at another service, whose diagnosis revealed reaction lymphoid hyperplasia and mature fat tissue with no atypias. A computed tomography (CT) with contrast of the neck revealed highly dense bilateral images, while an investigation of the cervical arteries through magnetic resonance imaging (MRI) showed hypersignal in T2 sequences, bilaterally. On the left, the lesion fully involved the internal and external carotids (Figures 1-2); arteriography of the carotid revealed a tumor blush in the common right carotid bifurcation and expanded angle. Presence of upper thyroidal artery branches and ascending pharyngeal artery led to an opaque-like imaging (Figure 3). A similar and smaller image in the contralateral carotid bifurcation was also observed. Bilaterally, brain blood flow was not altered.
Patient was submitted to selective right arterial embolization 24 hours before the surgical procedure, resulting in 90% reduction of tumor blood flow, except for irrigation of a small segment by carotid bifurcation direct branches.
The lesion was surgically removed along with the internal and external segments involved by tumor. Reconstruction was performed with an external saphenous vein flap (latero-terminal), reuniting the common and internal carotids. Hypoglossal nerve was damaged, as it was fixed to the tumor. Contralateral lesion was not approached at the same surgical procedure.
Postoperative recovery went well except for ipsilateral hypoglossal nerve paralysis.
DiscussionCarotid body paragangliomas are rare, benign, highly vascular slow-growing tumors of the neural crest arising from the paraganglionic tissue. The carotid body derives from both the mesoderm and third brachial arch elements and the neural crest ectoderm. It is usually located in the adventitious layer of the common carotid posterior-medial portion. Involvement of the middle layer is rare. These tumors are usually related to individuals residing in high altitude places5, suggesting that constant hypoxia stimulation may contribute to carotid body cellular hyperplasia 6.
Paraganglionic tumors may occur at any age, even though they are most frequently diagnosed in subjects between 45 and 50 years. Distribution by sex is differently described in the literature. Shamblim et al.7 have reported 69% male patients (62 and 90 years). Parry et al.3 studied 222 patients from 10 different institutions, in which 66% (146) of cases were women.
Carotid body tumors arise as a painless slow-growing mass on the neck carotid bifurcation, anteriorly to the sternocleidomastoid muscle border and laterally to the hyoid bone extremity. Upon palpation, tumor is horizontally mobile, vertically fixed and pulsatile. Large and invasive tumors may cause hoarseness, dysphagia and vocal weakness. Cranial nerve involvement occurs in about 20% of the cases, out of which the vagal and hypoglossal structures are the most affected ones8. Hypertension occurs in 6% of patients and has been associated with catecholamine secreted by tumors9. Approximately 2-10% are bilateral cases, either at initial or subsequent presentation 3,10,11. Bilateral tumors are seemingly to occur at earlier ages3.
Paragangliomas have been associated with thyroid medullar carcinomas and with patients with neurofibromatosis. Familial paragangliomas have also been reported, most commonly as bilateral carotid body tumors 5,10,11. Extra-adrenal paragangliomas, particularly of the head and neck region, presenting gastric leiomyosarcoma and pulmonary chondroma, have been denominated Carney's Syndrome.
Diagnosis of carotid paragangliomas may be obtained through selective arteriography, which may show the presence of a vascular mass in the common carotid artery bifurcation. Most authors contraindicate diagnostic biopsy due to bleeding risks. Neck computed tomography reveals an isodense mass; without contrast, the lesion shows hypodensity, which, after injection12, appears as a highly dense structure. In general, magnetic resonance imaging (MRI) presents an intermediate signal in T1 sequences and hypersignal in T2 sequences. Serpiginous images are frequently identified with no lesion signal in all image sequences, suggesting presence of dominant vessels, a feature called "salt and pepper"12-15. Hypervascular schwannoma 11 is the main differential diagnosis. Malignancy potential of carotid body tumors is questionable and the rate ranges from 1.5 to 50% in the literature 6,10,12. Disease metastatic evolution is usually extremely slow. The most common sites involved include lungs and bones11.
Treatment is mainly surgical. Relapses are very rare after tumor removal - approximately 10% of cases15. The most important improvement in surgery has been the recognition of the sub-adventitious plane and its dissection, allowing total tumor removal and carotid artery preservation. Sometimes this artery may be sacrificed during surgery, especially in large tumors with invasive or malignant behavior. A flap is rarely necessary to replace carotid bifurcation. Radiotherapy is not the treatment of choice, once these are radio-resistant tumors5.
In the presence of neck bilateral pulsatile horizontally mobile and vertically fixed mass, the diagnosis of carotid body paraganglioma must be considered, regardless of being a rare condition. In these cases, fine needle aspiration should be avoided due to risk of complications. Imaging examinations are relevant for diagnostic confirmation.
Our patient was submitted to resection of lesion along with involved parts of internal and external carotid arteries. Sometimes, sub-adventitious dissection is not feasible, even though it facilitates tumor resection, as tumor eventually infiltrates to other vessel layers, reaching the lumen. In the present reported case, tumor infiltration fully reached the arterial wall. Reconstruction was performed using an external saphenous vein flap, between the common carotid artery and the internal carotid.
Closing Remarks
A rare case of bilateral carotid paraganglioma is reported. Literature reveals that 2%-10% of the cases are family syndromes. Arteriography consists of a relevant diagnostic method, avoiding the risks of an incision biopsy. Surgical treatment remains the key therapeutic approach, using the sub-adventitious dissection approach when possible. The current available techniques, added to the surgeons' expertise, have provided excellent results with increasingly fewer neurological complications.
References
1. Farr HW. Carotid body tumors: a 40-year study. CA Cancer J Clin 1980; 30(5): 260-5.
2. Padberg Jr FT, Cady B, Persson AV. Carotid body tumor: The Lahey Clinic Experience. Am J Surg 1983; 145:526-28.
3. Parry DM, Li FP, Strong LC, Carney JA, Schottenfeld D, Reirner RR, Grufferman S. Carotid body tumors in humans: Genetics and epidemiology. J Natl Cancer Inst 1982; 68(4): 573-78.
4. Fries JG, Chamberlin JA. Extra-adrenal pheocromocytoma, literature review and report of a cervical pheocromocytoma. Surgery 1968; 63:268.
5. Thawley SE, Pange WR, Batsakis JG, Lindberg RD. Comprehensive management of head and neck tumors, 2 ed, Philadelphia, WB Saunders Company, 1999; 1345-49.
6. Hodge KM, Byers RM, Peters LJ. Paragangliomas of the head and neck. Arch Otolaryngol Head and Neck Surg 1988; 114(8): 872-77.
7. Shamblin WR, ReMine WH, Sheps SG, Harrison EG. Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg 1971; 122:732-39.
8. Davidge-Pitts KJ, Pantanowitz D. Carotid body tumors. Surg Annu 1984; 16: 203-27.
9. Fruin ME, Smoker WR, Harnsberger HR. The carotid space in the suprahyoid neck. Semin Ultrasound CT MR 1990; 11(6): 504-19.
10. Robertson DI, Cooney TP. Malignant carotid body paraganglioma: Light and electron microscopic study of the tumor and its metastases. Cancer 1980; 46(12):2623-33.
11. Sabiston Jr DC, Duke JB, Lyerly HK. Tratado de cirurgia - As bases biológicas da prática cirúrgica moderna, 15 ed, Rio de Janeiro, Guanabara Koogan, 1999; 1542-44.
12. High. Altitude chemodectoma. Lancet 1973; 1(7818):1493.
13. Carvalho MB. Tratado de cirurgia de cabeça e pescoço e otorrinolaringologia, 1ed, São Paulo, Atheneu, 2001; 138-139.
14. Farhood AI, Hajdu SI, Shiu MH, Strong EW. Soft tissue sarcomas of the head and neck in adults. Am J Surg 1990; 160(4): 365-9.
15. Lemaire M, Persu A, Hainaut P, De Plaen JF. Hereditary paraganglioma. J Intern Med 1999; 246(1): 113-6.
 Figure 1:
Figure 1: Cervical angioresonance. Axial section showing lesions with hypersignal in the right T2 sequences, bilateral and fully involving the internal and external carotid circumference.
 Figure 2:
Figure 2: Cervical angioresonance. Coronal section revealing a bilateral lesion.
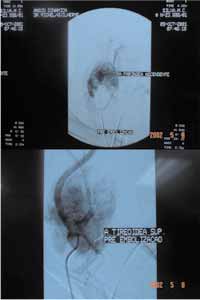 Figure 3:
Figure 3: Arteriography investigation of carotid arteries, showing tumor blushing in the right common carotid bifurcation. The opaque-like imaging is due to presence of upper thyroidal artery branches and the ascending pharyngeal artery. A similar and smaller image in the contralateral carotid bifurcation is also observed.


