IntroductionBasedow-Graves disease is the main cause of hyperthyroidism totaling about 85% of this affection. A common disease, with prevalence of about 0.3% in the population, it is a multi-systemic disease that affects the thyroid and normally has dermatopathy and ophthalmopathy. Eye involvement in Basedow-Graves disease is clinically diagnosed in about 30% of the cases, but in 90% of them it may be detected by computer tomography, ultrasound or magnetic resonance imaging 1.
Ophthalmic manifestations of Basedow-Graves disease are: palpebral retraction, proptosis, kemosis, diplopia, corneal exposure and optical neuropathy. These manifestations occur mainly by orbital content increase, through deposition of aminoglycans, fibrosis and edema, leading to venous congestion and prolapse of ocular globe to the anterior region, which presents less resistance 2.
In most cases, there is improvement of orbital compromise with hyperthyroidism treatment, be it through thyroidectomy, clinical treatment or radioactive iodine. However, in some cases there is no regression or some cases even progress to worsening of impairment.
Treatment of eye impairment depends on severity, staging, and clinical status of the patient, which may vary from simple clinical observation to treatment with antiinflammatory drugs, radiotherapy, immunotherapy and surgical intervention 3.
In the non-inflammatory stage, clinical treatment or radiotherapy produce dissatisfactory results, and we should prefer to correct the sequelae left by the scaring process: palpebral retraction, exophthalmus, and diplopia. In this stage, the main treatment is surgery, such as orbital decompression, correction of diplopia, correction of palpebral retraction and blepharoplasty. Orbital decompression is indicated in optical neuropathy, excessive proptosis, exposure ceratitis, glaucoma secondary to increase in intra-orbital volume, in disabling pain and to relieve from therapeutic effects of corticoid. Another indication is facial disfiguration, which causes major psychological and social disorders to the patient with exophthalmus 4.
The main forms of orbital decompression consist of removal of intra-orbital fat, removal of part of the orbital walls and expansion of orbital walls 4.
Dollinger in 1911 reported the first orbital decompression using orbitotomy of lateral wall by Kronlein incision, used to remove orbital tumors 5. Moore was the first to attract attention to the reduction of orbital pressure after reduction of its content: he removed orbital fat after conjunctiva incision on the inferior eyelid 6.
Walsh and Ogura, in 1957, combined anterior techniques and decompressed the orbit removing the inferior and medial walls through transoral maxillary antrostomy 7. This technique was popularized, being one of the most commonly used techniques by surgeons nowadays.
As a result of technology advance, endoscopy-assisted endonasal surgeries were developed. Kennedy in 1990 conducted orbital decompression by endonasal endoscopic access with removal of medial and inferior walls 8. Owing to expansion of drainage ostium of maxillary sinus and expansion of nasal-frontal recess using the endoscope, it is believed that it is possible to reduce the incidence of rhinosinusal infections compared to orbital decompressions without the endoscope 8.
This study aimed at reporting the incidence of acute and chronic rhinosinusitis after 12 months of follow-up post-orbital decompressions in patients with Graves ophthalmopathy submitted to removal of lateral and inferior orbital walls by external and medial access by endoscopy-assisted endonasal access, as advocated by the technique 9.
Material and MethodIn the period between April 2001 and May 2002, 16 patients with Graves ophthalmopathy from the ambulatory of the Sector of Orbit, Department of Ophthalmology, UNIFESP, were submitted to decompression of 18 orbits, after approval of the research project by the Research Ethics Committee, UNIFESP, N 288/01.
Ages ranged from 21 to 72 years, being that mean age was 45.1 years. Ten patients were female and six were male subjects (Table 1). Measurement of apoptosis was made by exophthalmus meter Hertel and ranged from 24 to 36mm, mean of 27.2mm. The postoperative follow-up ranged from 12 to 18 months.
We included patients that presented proptosis by Graves ophthalmopathy equal or greater than 24 millimeters and excluded the patients that presented ophthalmic signs of inflammation in the past six months, according to Clinical Activity Score 10, or clinical or radiological signs of rhinosinusitis.
We conducted 18 orbital decompressions being that 14 patients were operated on one single eye and two patients were operated on both. Thirteen surgeries were indicated owing to facial disfiguration caused by the disease, one patient presented primary glaucoma, and two had ceratitis.
All patients were assessed by the Discipline of Endocrinology, UNIFESP, and diagnosed as having Gravis ophthalmopathy, they were treated with corticoids in the inflammatory stage of the disease; four of them had also undergone eye radiotherapy.
In addition to endocrinological assessment, patients underwent ophthalmologic examination that comprised measurement of visual acuity using decimal optometric scale, computed visual field, assessment of eye fundus, ocular motility and diplopia. Proptosis was measured with exophthalmus meter Hertel and it was measured by one single observer during the whole study, and by CT scan.
In each case, we made photographic control, paranasal sinuses CT scan at axial and coronal sections, and rhinoscopy before and one year after orbital decompression.
Surgical techniquePatients were submitted to general anesthesia and one single orbit was operated per surgical time. The combined route of orbital decompressions consisted of two accesses, by external incision on the skin and endonasally 9.
We started by decompressing the orbit via external access, with an incision of modified blepharoplasty. Through the incision we removed the lateral and inferior walls, the latter medially removed from the infraorbital bundle.
In order to access the medial wall of the orbit, we used endonasal via, using rigid endoscope of 4mm with angulation of 0, 30 and 45 degrees.
We conducted wide sphenoethmoidectomy with expansion of the maxillary sinus ostium and identification of the frontal sinus ostium. Papyraceous lamina was removed in all its extension, and the periorbit was incised from posterior to anterior. Thus, the fatty body of the orbit went into the space created by the ethmoidectomy, having the middle concha as the limit.
ResultsNo patients presented symptoms of acute or chronic rhinosinusitis in the clinical follow-up and postoperative endonasal assessment.
Paranasal sinuses CT scan control 12 months after surgery showed three patients with maxillary sinus velamentum and one patient presented ipsilateral frontal sinus velamentum (Photos 1 and 2).
Table 1. Distribution of sample according to gender, age, race, and radiotherapy.
B - Caucasian
N - Black
M - Male
F - Female

Photo 1. Velamentum of right maxillary sinus.
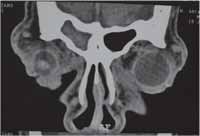
Photo 2. Velamentum of right frontal sinus.
The association of endoscopy in the orbital decompression surgery is made according to the paranasal sinuses surgical standardization 8, in which drainage ostium of maxillary sinus is expanded, nasal-frontal recess is opened and ethmoid and sphenoid sinuses are cleaned so that they do not obstruct ventilation and drainage of the sinuses; it is expected to have reduction in number of sinusitis cases after orbital decompression.
Warren (1989) in 305 orbital decompressions using Walsh and Ogura technique 7 reported 5 cases of rhinosinusitis efficiently treated with antibiotics 11.
Some authors demonstrated lower incidence of rhinosinusitis in the groups that had orbital decompression by endoscopy-assisted endonasal access compared to the group that had orbital decompression by external or transoral access 8, 12, 13, serving as a stimulus for the association of endoscopy-assisted endonasal surgery and external techniques, reducing postoperative complications 9, 14, 15.
It is quite difficult to assess the presence of acute rhinosinusitis after surgery, since the symptoms can be mixed up for symptoms caused by the surgical trauma. Imaging exams in the acute stage are not useful, since blood and edema hinder the assessment.
Twelve months after the surgery, CT scan evidenced maxillary and ethmoid sinuses partially occupied with orbital content, hindering radiological assessment.
The value of radiological CT scan findings in asymptomatic patients is discussable, since we did not find any studies in the literature correlating CT scan findings in asymptomatic patients submitted to orbital decompression and their clinical progression.
We decided to have clinical, endoscopic and paranasal sinuses CT scan follow-up in patients that were asymptomatic and with paranasal sinuses velamentum, but it is necessary to have further follow-up of these patients to better understand the variable of sinusal velamentum as predisposing factor for rhinosinusitis complications.
ConclusionThe combination of endoscopy-assisted endonasal access with external access in orbital decompression did not present clinically manifested rhinosinusitis complications, but the percentage of CT scan that presented paranasal sinuses velamentum (22%) was quite high.
References1. Villadolid MC, Yokoyama N, Izumi M, et al. Untreated Graves disease patients without clinical ophthalmopathy demonstrate a high frequency of extraocular muscle EOM enlargement by magnetic resonance. J Clin Endocrinol Metab 1995; 80:2830-3.
2. Gorman CA. Ophthalmopathy of Graves disease. N Engl J Méd 1983; 308:453-4.
3. Bartalena L, Pinchera A, Marcocci C. Management of Graves' ophthalmopathy: reality and perspectives. Endocr Rev 2000; 212:168-99.
4. Mouritis MP, Rose GE, Garrity J A, Nardi M, Matton G, Koornneef L. Surgical management of Graves' ophthalmopathy. In: Prumel MF. Recent developments in Graves' ophthalmopathy. Boston, Kluwer Academic Publishers, 2000. p.192.
5. Dollinger J. Die drickentlastlung der Augenhokle durch entfurnung der aussern Orbitalwand bei hochgradigen. Exophthalmos und Koneskutwer. Hornhauterkronkung. Disch Wochenschr 1911; 37:1888-90.
6. Moore R. Exophthalmos and limitation ofthe eye movements of Graves disease. Lancet 1920; 2:701.
7. Walsh TE, Ogura JH. Transantral orbital decompression for malignant exophthalmos. Laryngoscope 1957; 67:544-68.
8. Kennedy DW, Goodstein ML, Miller NR, et al. Endoscopic transnasal orbital decompression. Arch Otolaryngol Head Neck Surg 1990; 116:275-82.
9. Pezato R, Pereira MD, Manso PG, Santos RP. Three-wall decompression technique using transpalpebral and endonasal approach in patients with Graves'ophthalmopathy. Rhinology 2003; 41:231-4.
10. Mouritis MP, Koornneef L, Wiersinga WM. Clinical criteria for the assessment of disease activity in Graves' ophthalmopathy: a novel approach. Br J Ophthalmol 1989; 97:639-44.
11. Warren JD, Spector JG, Burde R. Long-term follow-up and recent observatins on 305 cases of orbital decompression for disthyroid orbitopathy. Laryngoscope 1989; 99:35-40.
12. Lund V, Larkin G, Fells P, Adams G. Orbital decompression for thyroid eye disease: a comparison of external and endoscopic techniques. J Laringol Otol 1997; 111:1051-5.
13. Maldonado AP, Ruiz RM, Aguayo AV, Mendez JAM, Garcia JFP, Lopez JG. Cirugía descompresiva de la órbita em pacientes com exoftalmos por Enfermedad de Graves-Basedow. Gac Mèd Mex 2000; 136:11-4.
14. Ulualp SO, Massaro BM, Toohill RJ. Course of proptosis in patients with Graves disease after endoscopic orbital decompression. Laryngoscope 1999; 109:1217-22.
15. Unal M, Ieri F, Konuk O, Hasanreisoglu B. Balanced orbital decompression combined with fat removal in Graves' ophthalmopathy: Do we really need to remove the third wall? Ophthal Plas Reconst Surg 2003; 192:112-8.
1 Post-Graduate studies under course, Discipline of Plastic Surgery, Federal University of Sao Paulo, Escola Paulista de Medicina, UNIFESP-EPM.
2 Post-Graduate studies under course, Discipline of Otorhinolaryngology, UNIFESP-EPM.
3 Master degree, head of the Sector of Orbit, Department of Ophthalmology, UNIFESP-EPM.
4 Professor, Ph.D., responsible for the Sector of Craniofacial Surgery, Discipline of Plastic Surgery, UNIFESP-EPM.
Study conducted at the Sector of Orbit, Department of Ophthalmology, UNIFESP-EPM.
Address correspondence to: Rogério Pezato - R. Napoleão de Barros 715, 4º andar, secretaria da Disciplina de Cirurgia Plástica.
Tel 0xx115576-4065 - E-mail pezatobau@ig.com.br
Article submitted ton December 18, 2002. Article accepted on April 14, 2004.


