IntroductionIn 1922 Vinson, from the Mayo Clinic, described the syndrome of pharyngeal dysphagia and anemia, frequently associated with splenomegaly in middle-aged women1, crediting to Plummer the recognition of this clinical entity, which became known as Plummer-Vinson syndrome. At the same time in England, Paterson-Brown-Kelly described a similar entity that received their names2, 3. Initially dysphagia was considered hysterical3 or caused by muscle spasms2 and in 1939, Waldenström described it as sideropenic dysphagia 4. Later, iron deficiency, atrophic glossitis, clubbing fingers, angular cheilitis, achlorydia and esophageal web were added to the syndrome.
The initial dysphagia is intermittent and become constant as the disease progresses. If treated early with iron replacement, the progression can be stopped, preventing formation of fibrosis caused by chronic inflammation of the esophageal mucosa that leads to esophageal web, which is initially anterior and then becomes a circumference with time. The association with iron-deficiency anemia and the characteristic clinical signs (angular cheilitis, atrophic glossitis, and normally achlorydia, liver and splenomegaly)confirm the diagnosis of Plummer-Vinson syndrome.
We report one clinical case of Plummer-Vinson syndrome started by dyspnea and adinamia, discussing the clinical findings, complementary exams and treatment.
CASE REPORTFemale, Caucasian 84 year-old patient, born and living in São Paulo, housewife, came to the emergency room with history of dyspnea after physical stress (such as walking from the bedroom to the living room) and adinamia for 1 week. She referred progressive dysphagia for the past 3-4 years, initially with solid foods, then with paste foods, followed by episodes of aspiration of food content and onset of lesions on the edges of the mouth and tongue, which presented periods of spontaneous remission. She reported loss of weight for the past 3 years, systemic hypertension and gastrectomy 40 years before owing to hemorrhagic ulcer.
At physical examination, the patient had general good status, paleness ¾+, hydrated and dyspneic. She had a supra-umbilical median longitudinal scar seen in the abdominal examination. At ENT examination, we detected glossitis with papillary atrophy and angular cheilitis (Figure 1).
Laboratory tests showed hypochromic microcytic anemia and abnormal serum iron and transferrin saturation: CBC - Hb: 7.8mg%, Ht: 25.2%, Mean globular volume (VCM): 65.8 (nl 80-100), Mean globular hemoglobin (HCM): 20.3 pg (nl 26-34), Mean globular hemoglobin concentration (CHCM): 30.8% (nl 32-36), Serum iron: 34 ng/dL (nl 40-150), Transferrin saturation: 8% (nl 20-50).
Barium swallow exam showed presence of an esophageal web on the proximal third of the esophagus (Figures 2 and 3). Upper digestive endoscopy revealed reduction of lumen and caliber of the organ at the level of the laryngeal vestibule and proximal esophagus, owing to the thick membrane that compromised the whole circumference of the esophagus; the remaining mucosa was intact.
The patient was submitted to blood transfusion, esophageal dilation and iron replacement and progressed well with total remission of symptoms of dysphagia and food aspiration.
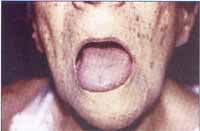
Figure 1. Oroscopy with glossitis.

Figure 2. Barium swallow exam showing narrowing.

Figure 3. Barium swallow exam showing narrowing.
The case report presented here had the classical characteristics of Plummer-Vinson syndrome, whose peak of incidence is in the 6th decade of life, with predominance in female patients. The clinical signs can be divided into minor and major, such as dysphagia, anemia, glossitis and laryngeal membrane as the major, and angular cheilitis, splenomegaly and achlorydia as the minor signs5.
The clinical history demonstrated progressive dysphagia associated with symptoms of iron deficiency anemia, however, only 10% of the patients with these symptoms develop post-cricoid web, usually associated with atrophic glossitis and angular cheilitis, leading to development of an autoimmune explanation to the pathophysiology6.
Clinical pathology characteristics are epithelial atrophy, hyperkeratosis, chronic submucous inflammatory infiltrate and degeneration and subjacent muscle atrophy. These abnormalities can be easily found in the tongue and oral mucosa, as well as in the hypopharynx, esophagus, nose, colon, rectum and vagina7, 8.
Laboratory findings demonstrate hypochromic microcytic anemia, reduction in saturation of transferrin and increase in total binding capacity of iron. Barium swallow exam with ionic barium contrast shows esophageal web, which can be also apparent in upper digestive endoscopy.
Plummer-Vinson syndrome is considered a precursor of post-cricoid cancer, with the peak of malignant transformation 10 years after the onset of the disease; the incidence of progression to carcinoma varies in the literature from 2 to 70%, and this variability is due to differences in treatment and in severity of anemia7, 9, 10. The malignization site is normally the area proximal to the web, possibly owing to chronic irritation of the mucosa.
Treatment consists of iron replacement therapy, blood transfusion if necessary to correct severe anemia, and esophageal dilation when dysphagia and esophageal web do not respond to clinical treatment or when they have been present for over two years5.
In the case reported here, the patient presented severe anemia, with significant clinical picture and advanced dysphagia, being treated with blood transfusion in addition to iron oral replacement; she was also submitted to esophageal dilation to have quicker improvement of dysphagia.
Closing remarksPlummer-Vinson syndrome is a rare clinical entity with different otorhinolaryngological symptoms such as dysphagia, atrophic glossitis and angular cheilitis, among others, which deserves extra-careful attention because of its potential for malignant transformation in the post-cricoid region, a site of poor prognosis in head and neck cancer.
References 1. Vinson PO. Hysterical dysphagia. Minn Med 1922;5:107.
2. Kelly AB. Spasm at the entrance of the esophagus. J Laryngol Rhinol Otol 1919;34:285.
3. Paterson DR. A clinical type of dysphagia. J Laryng Otol 1919;34:289.
4. Waldenström J, Kjellberg SR. The roentgenological diagnosis of sideropenic dysphagia. Acta Radiol 1939;20:618.
5. Mansell NJ, Jani P, Bailey CM. Plummer-Vinson syndrome: a rare presentation in a child. J Laryngol Otol 1999 May;113:475-76.
6. Geerlings SE, Statios van Eps LW. Pathogenesis and consequences of Plummer-Vinson syndrome. Clin Investigator 1992;70:629-30.
7. Entwhistle CC, Jacobs A. Histological findings in the Paterson Kelly syndrome. J Clin Pathol 1965;18:408-13.
8. MacNab-Jones RF. The Paterson, Brown-Kelly syndrome: its relationship to iron deficiency and post cricoid carcinoma. J Laryngol Otol 1961;75:529-61.
9. Adams GL. Malignant tumors of the larynx and hypopharynx. In: Cummings, CW et al. Otolaryngology, Head and Neck Surgery, 3a edição, Saint Louis: Mosby-Year Book Inc.; 1998. p.2131-2175.
10. Chilholm, M. The association of webs, iron and post-cricoid carcinoma. Postgrad Med J 1974;50:215-19.
1 Resident Physician in Otorhinolaryngology, Federal University of São Paulo - Escola Paulista de Medicina-UNIFESP.
2 Otorhinolaryngologist.
3 Full Professor, Federal University of São Paulo-UNIFESP, Head of the Discipline of Pediatric Otorhinolaryngology, Escola Paulista de Medicina-UNIFESP.
Affiliation: Escola Paulista de Medicina – Federal University of São Paulo – Department of Otorhinolaryngology and Human Communication Disorders.
Address correspondence to: Fernando Danelon Leonhardt – R. Bandeira Paulista, 142 apto. 22
04532-000 – São Paulo – SP
Tel. (55 11) 3168-0103 – E-mail: fernandodanelon@uol.com.br
Article submitted on October 22, 2001. Article accepted on December 13, 2001


