The lop, prominent or protruding ear is a deformity characterized by those abnormalities which may occur singly or in combination:
1 - Underdevelopment of antihelix
2 - Overdevelopment of conchal cartilage
3 - Increased angle between the pinna and the scalp: (Normal angle is 25° to 30°).
4 - Lobule protrusion
It is a hereditary malformation transmitted as a Mendelian dominant Potter 1937, Rogers 19681. Many times it may induce psychological problems because the children with this type of deformity are often ridiculed by their peers. The external ear reaches its growth near completion in childhood. It is safe to correct those malformations in the pre-school age. We prefer to operate between ages of four to six. It is important to examine carefully the patient preoperatively and establish the nature of the deformities in each individual case. This is done with attention to the consistency of the auricular cartilage by folding the ear against the scalp. The treatment is then planned accordingly.
Embryology
Earlier authors stated the first branchial arch (mandibular) gives the hillocks 1, 2, and 3 for the formation of tragus, helix and crus helicis. The antitragus, antihelix and lobule comes from the hillocks 4, 5, and 6, derived from the second branchial arch (hyoid). Mote recently, investigators have concluded that the auricle with the exception of the tragus comes from the second branchial arch. If during the 12th to 16th weeks of gestation the antihelix fails to Unfold, the helix continues to- overhang and prottusion will persist resulting in lop ear.2
History and Literature ReviewThe first surgeon to devise an operation to correct the lop ear was Dieffenbach (1845) 3 in Germany. The surgical technique consisted of excision of the retroauricular skin and suture of the auricular cartilage to the mastoid periosteum. Ely (1881) 4 of New York was the first to remove the skin and cartilage. Monks (1891) and Morestin (1903) modified Dieffenbach's and Ely's techniques by excision of the skin and cartilage. Luckett (1910) 5 ser forth the concept that the absence or underdevelopment of the antihelix was the essential cause of the deformity. Davis and Kitlowski in 1937 tried to correct the deformity by breaking the cartilage spring. Young in 1944 introduced the concept of removal of the cartilage strip and excision of elliptical segments of the antihelix. Becker in 19496 published a very important paper introducing an original technique which is the basic concept of modera otoplasty. It consists of incisions, excision of the cartilage, removal of the cauda helicis, and application of sutures. This technique was later modified by Converse et al in 19557. Farrior (1959)8 proposed a method of excising longitudinal wedges of cartilage without removing the full thickness of the cartilage. These strips were removed along the antihelix. to break the spring, producing adequate convexity. Horizontal mattress sutures were used to secure permanent shape of the newly-formed antihelix. Mustarde (1963)9 introduced the simple mattress-suture technique without cartilage excision. Later Holmes, Senstrom, Furnas, Feuerstein, Webster, Wright, Nachlas et al, Gay and others suggested further modifications of these techniques.10, 11, 12, 13, 14
Surgical Technique
The operative procedure is begun by making an incision on the posterior surface of the ear beginning superiorly. It follows the helical rim in a circumlinear fashion. It is made approximately 1 cm. from the free edge of the helix. The skin to be removed is determined by folding the ear on itself and noting the redundancy that is present. This skin is then removed by an incision which is the mirror image of the first. This is made above the posterior auricular sulcus, removing a portion of the skin which is elliptical in shape. Thus the skin is then elevated and removed completely, using the plane between the subcutaneous tissue and the perichondrium. Following this, with Stevens scissors, skin flaps are developed by sharp and blunt dissection undermining up to the helical rim and down to the posterior auricular sulcus. It is undermined extensively and all ligamentous and muscular attachments are severed in the sulcus, down to the mastoid periosteum. Hemostasis is accomplished using elettrocautery. At this time, the new antihelix is mapped out. The ear is folded upon itself to the desired position, forming the new antihelix. Using a straight Keith needle threaded with 4-0 black silk the first marking suture is placed on the anterior aspect of the auricle, just superior to the inferior crus. A bare Keith needle is introduced from the anterior aspect just superior to the superior crus, created by the folding of the ear, perforating the cartilage posteriorly. Then the threaded needle is introduced into the tract created by the bate needle, as it is withdrawn. This, thereby, completes the loop on the posterior surface of the auricular cartilage. Two to four more silk-marking sutures are placed along the edges from superiorly to the cauda helix, to complete the marking of the new antihelical outline. Following this outline, a wire brush attached to a Stryker hand piece is then utilized to score and thus weaken the cartilage. During this step, care must be taken to avoid entangling the sutures within the wire brush. To accomplish this, the sutures may be looped out of the field by increasing their slack or even cut and retracted away from the wire brush. The perichondrium is left intact purposely in order to maintain blood supply to the cartilage. It is removed with the wire brush only in the areas where the cartilage is to be weakened. Care must also be taken to thin the cartilage as evenly as possible and to avoid perforating the cartilage and damaging the soft tissues on the anterior surface of the ear. The degree of weakening of the cartilage is determined by the amount of spring originally present and the amount of antihelix already formed. (Fig. 1). The next step is to obtain Keith needles without any suture material and place them at the superior and inferior most extent of the concha. These are placed where the concha meets the newly-formed antihelix. The Keith needles are advance posteriorly. At this time, using methylene blue, a crescent-shaped piece of cartilage is outlined with its convexity towards the helical rim. The amount of. cartilage removed here is again determined by the excess of conchal cartilage present. (Fig. 2) Using a #15 blade, the conchal cartilage is then removed, care being taken to avoid injury to the anterior soft tissues. When the cartilage is removed, the spring of the conchal cartilage should be reduced enough so that the ear will lie in a desired position. If this is not the case, scissors may be used to weaken the cartilage further by extending the incision into that portion of the cartilage, towards the skull, which was not incised previously.
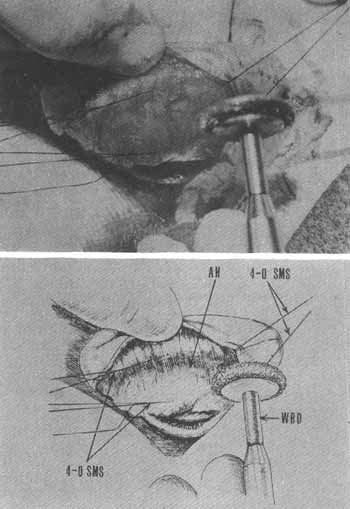
FIG. 1 - POSTERIOR ASPECT OF AURICULAR CARTILAGE WITH
ANTIHELIX MAPPED OUT.
AH = Antihelix: 4-0 SMS = 4.0 Silk Marking Sutures; WBD = Wire Brush Drill
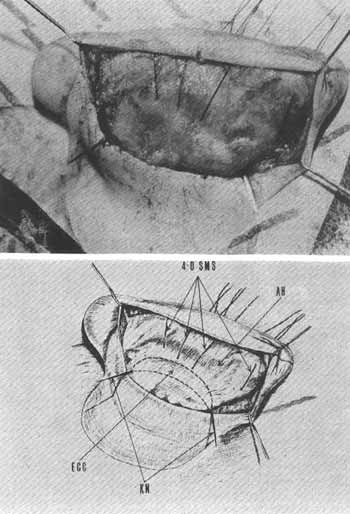
FIG. 2 - SHOWS 4 MARKING SUTURES OUTLINING THE NEW. ANTIHELIX. THE 2 KEITH NEEDLES INTRODUCED FROM ANTERIORLY HELP TO DEMARCATE THE INFERIOR AND THE SUPERIOR MOST EXTENT OF CONCHA TO BE REMOVED.
AH = Antihelix; ECC = Excessive Conchal Cartilage; 4-0 SMS = 4-0 Silk Marking Sutures; KN = KPIfh NPPd IPt
When the amount of spring has been reduced, the cartilage is trimmed so that there are no sharp edges at the corners of these incisions. Also, it is often necessary to remove a small triangular piece of conchal cartilage in order to obtain the desired position of the auricle. (Fig. 3) The skin on the anterior surface of the conchal cartilage is then undermined with scissors so that the redundant skin may drape properly, therefore avoiding post operative skin fo1ds. At this point, the cauda helicis is freed from the surrounding tissues and is trimmed from the helical rim as necessary to correct any deformiry which may be present at the lobule or inferior end of the helix. When all these steps have been completed, the ear may possibly lie in the desired position without any undue tension. The antihelix which has been created is now maintained and enhanced, if necessary, by the use of 4-0 clear monofilament nylon sutures. The sutures are placed in a horizontal mattress fashion, bow-stringing across the newly-formed antihelix on the posterior surface. They are placed from the scaphoid to the conchal side of the antihelix. Care must be taken, at this point, to include the perichondrium on the anterior surface of the ear in the suture. (Fig. 4) To facilitate this, the skin overlying the anterior surface of the antihelix may be elevated by the injection of normal saline into the subcutaneous layer. Beginning at the superior crus of the antihelix, approximately 3-5 of these sutures are applied, spacing them accordingly. Sequentially, as the 4-0 nylon horizontal mattress sutures are applied, the 4-0 silk marking sutures are removed. Each suture is tied down individually, the surgeon judging the amount of tension by the configuration of the antihelix which he desires to produce. (Fig. 5) The initial knot is a surgeon's knot followed by 4-5 simple knots with the final knot being applied with some pressure in order to lock it in place. Here again, the antihelix must be scrutinized to insure its proper configuration. Upon completion of this step, a nice antihelix should be present. A single 4-0 chromic suture is then applied from the midportion of the antihelix to the soft tissue medial and posterior to the concha, preferably to the mastoid periosteum. This is a singly applied suture which maintains the ear in a desired position. In cases where concha need not be removed, the technique consists only of horizontal mattress suture placement. Often, in young children the cartilage is so thin that scoring is not necessary.
A rubber-band drain is then inserted into the wound from its superior aspect along the soft tissues to exit inferiorly. A 4-0 silk suture applied to this rubber band is used during the post operative period to remove the drain from under the dressing. The rubber-band drain is not sutured to the soft tissues. When this is completed, the skin incision is closed posteriorly with 5-0 nylon interrupted sutures. A single 4-0 nylon vertical mattress suture is applied to the skin of the posterior auricular sulcus, down to the mastoid periosteum, to avoid blunting of the sulcus. The dressing consists of cotton soaked in mineral oil which is conformed to the newly-created antihelix and concha, thus filling all the crevices and folds of the ear. A bulky fluff dressing is then applied in the sulcus and over the ear. Care must be taken that the silk suture which is attached to the rubber-band drain is outside the dressing. The post-operative care is as follows: Two days postop the rubber-band drains are removed. Four days postop, the dressing is changed, care being taken not to disturb the coton that was placed in the operating room. The ear is inspected and a new lighter dressing is loosely applied. This new dressing is left until one week postop at which time it is removed along with the cotton packing and the post-auricular sutures. An appropriately-sized stockinette is applied during the second postop week, and is worn 24 hours a day. During the third and fourth weeks postop, the patient wears the stockinette only at night, and after this, requires no further dressings.
Case MaterialAll patients operated on had lop ear secondary to an absent or underdeveloped antihelix and/or excessive conchal cartilage. Other types of external ear deformities are not included in this study. From 1968 to 1974, we have operated on 61 patiens. Twenty-nine of these were our own private patients, and 32 were non-private, resident cases, done under our direct supervision and assistance at the Manhattan Eye, Ear and Throat Hospital, New York Medical College Metropolitan Hospital Center, Brooklyn Eye and Ear Hospital and the University of Miami Medical Center.. All patients were admitted to the hospital. General anesthesia was usually used with endotracheal intubation. Adults and teenagers often were done under local anesthesia, with adequate preoperative sedation. Four patients had unilateral deformity. The total number of ears was 118; 76.2% were children and teenagers from 4 to 15 years of age. On 37 ears, the technique used was horizontal-mattress sutures only with or without scoring of the cartilage. On most of our .cases (71) , however, we preferred the cartilage excision-incision with mattress sutures technique as described. The suture material used was mainly 4-0 monofilament clear nylon.
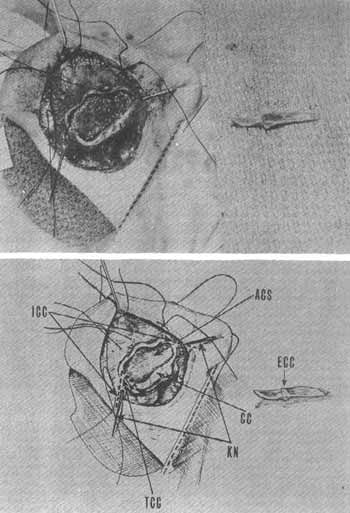
FIG. 3 - ECC = Excessive Conchal Cattilage (Removed); ICC - Incision Conchal Cartilage (To furthet break the spring); TCC ? Triangle Conchal Cartilage (To further obtain the desired position of auricle); ACS = Anterior Conchal Skin; CC = Conchal Cartilage; KN = Keith Needles.
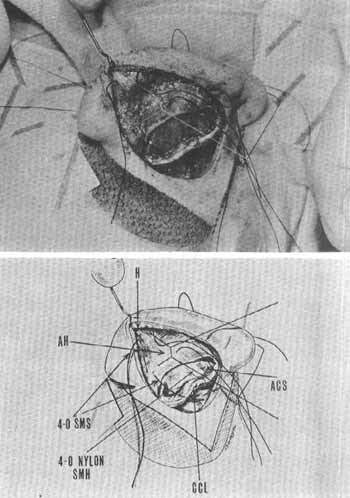
FIG. 4 - THE NEWLY CREATED ANTIHELIX IS MAINTAINED AND ENHANCED WITH HORIZONTAL MATTRESS SUTURES.
H = Helix; AH = Antihelix; 4-0 SMS = 4-0 Silk Marking Sutures; 4-0 Nylon SMH = 4-0 Nylon Suture Mattress Horizontal; ACS = Anterior Conchal Skin; CCL - Conchal Cartilage Lateral Aspect.
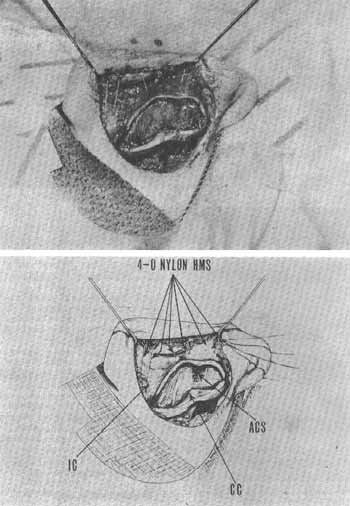
FIG. 5 - HORIZONTAL MATTRESS SUTURES USED (TOTAL OF 3 IN THIS CASE) TO MAINTAIN AND ENHANCE THE NEW ANTIHELIX.
4-0 Nylon HMS - 4-0 Nylon - Horizontal Mattress Sutures; IC = Inferior Crus; CC = Conchal Cartilage; ACS = Anterior Conchal Skin.
Mersilene and dacron were occasionally used. We prefer monofilament nylon because it produces practically no tissue reaction Piachke et al, 197115. Of the 118 ears, 100 (84.7%) healed well without infection or other complications. The typical lop ear deformities with underdeveloped antihelix and excessive conchal cartilage are shown in Figures 6, 7, 8. Postoperative pictures (Figures 9, 10, 11) demonstrate the results obtained with this technique.
ComplicationsThe type of complications and their incidence are reported in Table I. Ali skin infections were of a minor nature and responded well to systemic and topical antibiotics and warm saline soaks to the ear. Hematomas were evacuated using a clamp inserted through the suture line and then applying pressure. One mattress suture was extruded without infection, two months postoperatively. Two patients developed keloids, bilaterally, on the posterior auricular scar. One of them was treated with Kenalog injections with improvement. The other was lost to follow-up. No perichondritis ever occurred in our series. Prophylactic antibiotics (Ampicillin or Erythromycin) were used in all patients, for 7 days postoperatively.
Unsatisfactory Cosmetic Results I
In Table I the unsatisfactory cosmetic results are reported. Recurrent auricular protrusion occurred in 3 ears. Two were revised with good cosmetic results. One male adult had unilateral recurrence of protrusion but refused further surgery because he felt that the cosmetic result was somewhat better than his preoperative deformity. Over-correction occurred in 3 ears but no revisions were performed. One female adult had a minimal notching of her helix, which required no revision. The type of complications and unsatisfactory cosmetic results are similar to those reported by other authors. Goode et al, 1970; Feuerstein, 197416, 17.
TABLE I
Of our 118 ears 94.1 % had a good cosmetic postoperative result, pleasing either to the patient, the patient s family, or to the surgeon. The selection of technique, either mattress sutures, or cartilage excision-incision and mattress sutures, is based on the pre-operative evaluation with particular attention to the consistency of cartilage, underdevelopment of antihelix, and excess of the concha. The technique is derived from various sources with soma minor personal modifications. It is easy to learn and especially useful in the training of residents.
SummaryThe authors report their experience in the surgical treatment of 61 patients with lop, prominent, or protruding ears. Four patients had a unilateral deformity. The total number of operated ears was 118. The procedure used in 71 years consisted of a cartilage excision-incision and horizontal mattress suture technique. In 37 ears, horizontal mattress sutures with or without scoring of cartilage was used. The complications and unsatisfactory cosmetic results are reported. In conclusion, 94.1% of all cases had a good cosmetic result. The techniques are easy to learn and very useful in resident training.
ResumoOs autores relatam sua experiência no tratamento cirúrgico estético de 61 pacientes com deformidade congênita (tipo abano), da orelha externa. 118 orelhas foram operadas, sendo 4 casos de deformidade unilateral. Em 71 orelhas a técnica usada foi excisão-incisão de cartilagem e sutura tipo "U" horizontal. As outras 37 orelhas foram operadas usando somente a técnica de sutura tipo "U" horizontal com ou sem adelgaçamento da cartilagem. As complicações e resultados estéticos não satisfatórios são apresentados. A conclusão final é que 94,1 % dos casos relatados obtiveram resultados estéticos bons. Ambas técnicas são fáceis de apreender e muito úteis no treinamento de residentes.
References:1. Rogers, B. D.: Microtic, Lop, Cup and Pro truding Ears: Four Direct1y Inheritable Deformities. Plast Reconstr Surg 41: 208-231, 1968.
2. Anson, B. l.: Human Anatomy. Morris' Human Anatomy, 12th Ed. New York: McGraw-Hill Co., 1966.
3. Dieffenbach, J. F.: Die Operative Chirugie, Leipzig: F. A. Brockhaus, 1845.
4. Ely, E. T.: An Operation for Prominence of the Auricles. Arch Ophthal Oto 10: 97, 1881.
5. Luckett, W. H.: A New Operation for Prominent Ears Based on the Anatomy of the Deformity. Surg Gynec Obstet 10:635-637, 1910.
6. Becker O. J.: Surgical Correction of the Abnormally Protruding Ear. Arch Otol 50:541, 1949.
7. Converse, J. M., Nigro, A., Wilson, F. A., et al: A Technique for Surgical Correction of Lop Ears. Plast Reconstr Surg 15:411-418, 1955.
8. Farrior, R. F.: A Method. of Otoplasty. Arch Otol 69:400-408, 1959.
9. Mustarde, J. C.: Correction of Prominent Ear Using Simple Mauress Sutures. Brit J Plast Surg 16:170-176, 1963.
10. Holmes, E. M.: Otoplasty. Arch Otolaryng 83: 156-157, 1966.
11. Feuerstein, S. S.: Combined Technique of Oto-plasty. Laryngoscope 79: 1118, 1969.
12. Nachlas, N. E., Duncan, D., and Trail, M.: Otoplasty. Arch 0161 91: 44-49, 1970.
13. Wright W. K. Otoplasty Goals and Principies. Arch Otol 92:568-572, Dec. 1970.
14. Gay, E. C. Ir.: Auricular Repositioning Oto-plasty. Laryngoscope 84: 468-484, March 1974.
15. Pischke F. J. and Bortnick, E.: Experimental Otoplasty Using Rabbit Ear. Arch Otol 94: 220-223, 1971. Concludes - Clear monofilament nylon was the easiest suture material to handle and also produces the least amount of inflammatory reaction.
16. Goode, R. L., Proffitt, S. D. and Rafaty, M. F.: Complications of Otoplasty. Arch Otol 91:352-355, 1970.
17. Feuerstein, S. S.: Revision Techniques in Otoplasty. Evaluation and Management. Otolaryng Clin N. Amer 7 (1): 133-144, Feb. 1974.
* From the Department of Otolaryngology, University of Miami School of Medicine, Miami, Florida.
** From the Department of Otolaryngology, New York Medical College, New York, New York.


