INTRODUCTIONAbscesses localized in the encephalic region (brain and cerebellum) are neurological diseases with clinical manifestations that may vary in severity, from simple headache at initial stages to severe affections, with signs of intracranial hypertension, and at later stages, transtentorial herniation.
Early diagnosis, location of abscess and primary focus, which may be located close or far away, are essential for definition of management. ENT diseases are undoubtedly the most common cause of encephalic abscesses; among them, otogenic focus amounts to 30% to 40% (Cawthorne, 1945; Garfield, 1969; Ayyagari et al., 1982).
Since the initial studies with cerebral abscess, it is known that the mortality rate is worrisome, because the lesion is particularly known for its lethal potential (Morgan et al., 1973). Two very distinct treatment periods may be drawn: the first is the pre-antibiotic era, in which mortality rates varied from 60% to 80%, and the second post-antibiotic era, dropping the rates to 20% to 40% (Proctor, 1966; Wright and Grimaldi, 1973).
As a result of the development of more precise diagnostic tools, such as computed tomography (CT scan) and magnetic resonance imaging (MRI), early diagnosis now is possible with definition of the exact location of the lesion, in addition to postoperative monitoring of the patients (Rosenbloom et al., 1978; Whelan and Hilal, 1980; Leiberman et al., 1994).
Many different surgical approaches for cerebral abscesses have been described. The most frequently used technique is classic neurosurgical approach through craniotomy and/or trepanation (Vincent, 1938). However, the main debate has evolved around the treatment of the primary focus, that is, the otitis media, with performance of mastoidectomy during the existence of the otogenic abscess, followed by drainage through transmastoid route (Karamitsos et al., 1982).
Despite the use of antibiotic therapy, new surgical techniques and recent diagnostic methods, mortality and neurological sequelae rates are still high (Gower and McGuirt, 1983; Bradley et al., 1984).
As shown in the study by Penido et al., 1990, and Penido's dissertation thesis in 1992, plain drainage of the abscess is not the ideal intervention, because patients present recurrence of the process until resolution of the primary focus (in general, cholesteomatous otitis media). In view of these observations, we have conducted mastoidectomy to treat the primary focus with abscess drainage via transmastoid access, and sometimes though stereotactic route or trepanation, but always removing the infections focus from the mastoid.
The purpose of the present study was to assess evolution of otogenic encephalic abscess treatment in a 12-year period.
MATERIAL AND METHODThe present study comprised 25 cases of otogenic encephalic abscess followed up from October 1987 to March 2000 (12 years) in our service.
All patients were initially seen-in the Emergency Room, some by neurosurgery, others by otorhinolaryngology, and other by the pediatric department. In some cases, initial diagnosis was encephalic abscess with no location of primary focus. Patients had been submitted to clinical antibiotic therapy and some to drainage of the abscess by trepanation, but considering the poor clinical progression, the cases were referred to ENT assessment.
All patients were submitted to ENT examination and we detected cases of cholesteomatous chronic otitis media (CCOM) or acute otitis media (AOM), all of them with encephalic abscess confirmed by CT scan.
In patients that were in good clinical conditions, that is to say, those who had preserved level of consciousness, we performed preoperative pure tone audiometry. After the confirmation of the otogenic encephalic abscess, we chose to perform surgery in all cases of CCOM. We performed ample mastoidectomy, radical in most of the cases, with drainage of the abscess in the same surgical time, some through the same transmastoid route and others through stereotactic punch and emptying of the abscess.
The progression of patients was followed by a multidisciplinary team comprising infectious disease intensivists, neurosurgeons and otorhinolaryngologists.
RESULTSIn the 12-year period, there were 25 cases of otogenic encephalic abscesses, whose individual description is presented in Table 1.
Fourteen patients were males (56%) and eleven patients were females (44%). Ages ranged from six months to 71 years, and 72% of them (18 patients) were younger than 30 years and 48% were younger than 20 years. Intracranial abscess was secondary to CCOM in 20 cases (80%) and to AOM in 5 cases (20%). Patients with CCOM took in average 13 years from onset of otitis symptoms to onset of the abscess, ranging from a minimal of 6 months to a maximum of 40 years.
As to location of abscess, 19 cases (76%) were in the temporal lobe and six cases (24%) were in the cerebellum, 60% affecting the right hemisphere and 40% the left cerebral hemisphere.
Complications associated with the abscess were very common and some subjects had more than one complication. The most common abscess-related complication was meningitis, present in 14 cases (56%), followed by peripheral facial paralysis (12%), subdural empyema in two cases (8%), two cases of septicemia (8%), one case of lateral sinus thrombosis (4%) and one case of epidural empyema (4%).
We managed to perform abscess cultures of 22 cases, and 13 of them (59%) did not show bacterial growth. In five cases (23%), there was growth of Proteus Mirabilis; in one case (4.5%), Pseudonoma Aeruginosa; in one case (4.5%), Enterococos sp; in one case (4.5%), Pneumoccocus; and in one case (4.5%), Haemopbilus.
Audiometry was conducted in 15 cases and among them, 66% or 10 cases had conductive hearing loss, 20% (3 cases) had anacusis, one case (6%) had normal audiometry and one case (6%) had mixed hearing loss.
All patients were submitted to antibiotic clinical treatment. Out of 25 cases, 19 had been initially submitted to trepanation, with drainage of the abscess, and among them 11 patients (58%) had experienced recurrence, with quick recovery of the abscess, before its resolution. The six remaining patients did not undergo neurosurgical intervention because in 5 cases, mastoidectomy was chosen and followed by drainage of the abscess through transmastoid route, resulting in resolution of the process in all cases. One patient died because there had not been enough time to intervene.
Out of 25 cases, 19 were submitted to mastoidectomy (16 radical mastoidectomies and three conservative mastoidectomies) and in 12 cases, in addition to mastoidectomy, the abscess was drained through transmastoid route. These 12 patients did not present recurrence of the abscess, but there was recurrence of the cholesteatoma in two cases one year after surgery. In the other seven cases submitted to mastoidectomy, the approach of the abscess was performed by the neurosurgeon together with the otorhinolaryngologist or through separate stereotactic route. The six patients who did not undergo surgical ENT treatment, that is mastoidectomy, included 4 cases of AOM, who had no indication for surgery, and two other cases of CCOM that died before being assessed by the otorhinolaryngological team.
All cases whose primary focus was approached did not present recurrence of the abscess.
Throughout the 12 years, there has been a progressive change in the surgical intervention approach. Initially, patients were submitted to neurosurgical treatment and after poor results of trepanation or craniotomy they were referred to the otorhinolaryngologist. Then, mastoidectomy was performed. Recently, if there is hypothesis of otogenic abscess, the otorhinolaryngologist is immediately called and some surgeries are conducted together, in which the neurosurgeon focus on the abscess and the otorhinolaryngologist approaches the mastoid, in the same surgical act.
We reached mortality rate of 12% (3 cases) and 32% (eight cases) of neurological sequelae.
We also noticed that with the approach of the primary focus, the resolution of the process becomes much quicker, reducing the length of stay because there is no recurrence of abscess.
DISCUSSIONIntracranial complications of acute or chronic otitis media are extradural abscess, thrombophlebitis, meningitis, subdural empyema and cerebral and cerebellar abscesses (Goycoolea and Jung, 1991).
In the present study, we selected only cases of encephalic abscesses with or without associated complications. Some authors consider encephalic abscesses as the most frequent complication of otitis (Quijango et al., 1998, Wright and Grimaldi, 1973), whereas other statistics, such as the ones presented by Gower & McGuirt, 1983, and Habib et al., 1988, meningitis is the most common complication.
In the pre-antibiotic era, the overall percentage of intracranial complications of otitis media was 3%, and it has dropped to 1 % currently (Fernandez et al., 1987), in which cerebral abscess amounts to 0.3% of the cases (Harter, 1985). There has also been an inversion in facts, because now the most important cause is CCOM (Ballenger, 1988). This observation is confirmed by the present results, in which 80% of the encephalic abscesses were caused by CCOM.
We noticed that abscesses located in the cranial middle fossa (temporal and temporal-parietal lobes) were the most frequent ones, presenting a proportion of 19 to 6, located in the posterior fossa, as confirmed by the literature (Kaplan, 1985). This result may be explained by the fact that the dissemination of the infectious process to the central auditory system takes place by direct contamination and not through vascularization. In addition, the origin of the cholesteatoma is the attic region closer to the middle fossa, and the dura mater has higher adherence on the posterior fossa, impairing the formation of an abscess (Ballenger, 1988).
As to gender, there was a discreet predominance of males: 56% (14 cases) against 44% (11 cases), data in accordance with the literature that reports predominance of male patients (Habib et al., 1988).
The most affected age range is of young adults and we found 48% of the cases in patients below 20 years of age; we also detected 72% of the patients below the age of 30 years, in accordance with the data provided by other studies (Gower and McGuirt, 1983, Habib et al., 1988).

Figure 1. Pre-operative cerebellar abscess.
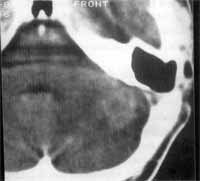
Figure 2. Total regression of post-mastoidectomy abscess and drainage of abscess through the same route.
A fact that called our attention was that the patients presented various years of progression of the COM with othorrea before the development of intracranial complications. If we calculate the age of patients at onset of otitis, we will realize that it has started at pre-school or school age, and the early the otitis the quicker the progression. In cases of cholesteatomas, the interval between onset of symptoms and onset of abscess was 13 years in average.
Other associated complication were also present and meningitis was the most common one, present in 56% of the cases; in a smaller number of cases there was facial paralysis, subdural empyema and thrombophlebitis. In some patients, it was not possible to perform CSF puncture because of the risk of transtentorial herniation, although they presented signs of meningeal irritation at clinical examination, which suggested that the association might be even more frequent.
The criteria for selection of use of antibiotic was initially adopted without the result of the culture based on the studies by Ayyagari et al., 1983, and Kangranarak et al., 1993, who demonstrated that the etiological agent responsible for encephalic abscesses were in most situations polymicroorganisms, both aerobic and anaerobic. We had a high percentage of sterile cultures and this fact may be explained by the perception that these patients had been previously taking antibiotics. In the cultures in which we isolated the agent, we detected a higher percentage of Proteus mirabilis; and we also isolated one case of Pseudomonas, and another of Enterococos sp, an anaerobic germ. We believe that our low? level of anaerobes is due to technical flaws during collection of materials, because they were collected sometimes during the night or weekends and were to be processed hours later.
As to analysis of audiometry, we observed that 20% of the cases of anacusis were on the side of the abscess, explained by the formation of a fistula on the lateral semicircular canal, because of the destruction caused by the cholesteatoma, which was later confirmed in the surgery in two cases. In one case, the patient had AOM and normal audiometry. However, most of the patients 66% presented conductive hearing loss, which is expected in middle ear infectious processes.
The use of CT scan is extremely useful in diagnosis and treatment of encephalic abscesses (Figures 1 to 5). It provides the definition of the exact site of lesion, early diagnosis and monitoring of therapeutic efficacy. The different CT sections - axial, coronal and sagittal, provide a three-dimensional visualization of the lesion, precisely determining dimensions and location of abscesses.
Based on the analysis and follow-up of the 25 patients, we noticed that initially they were submitted only to trepanation and craniotomy, without approaching the primary focus; there was a higher rate of recurrence of the cerebral infectious process, leading to neurological sequelae and longer length of hospital stay, even with administration of high doses of intravenous antibiotics. Conversely, patients that underwent mastoidectomy and drainage of the abscess right at diagnosis presented resolution of the case and reduced length of hospital stay, presenting few neurological sequelae. Therefore, we believe that the approach of the primary infectious process is essential to have successful results.

Figure 3. Preoperative temporal abscess.

Figure 4. Temporal abscess showing multiple sites.
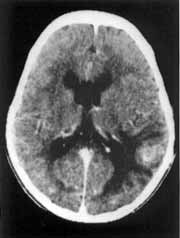
Figure 5. Total regression of post-mastoidectomy abscess and abscess drainage through the same route.
Another extremely important factor is early diagnosis and timely intervention.
Multidisciplinary approach of these patients with otorhinolaryngologist, neurosurgeon and infectologist has shown a significant improvement in the results.
The mortality rate of the pathology is still high: according to Matheus and Marus, 1988, it is 13.5%, and according to Kangsanarak, 1993, it is 18.6%. In our sample, it was 12% and we do believe that it was a result of more clinical investigations and primary focus intervention.
It is important to point out that patients who were at poor general status at the beginning of treatment, presenting severe headache, mental confusion and varied neurological symptomatology, showed promising prognosis few days after the ENT surgery, presenting quick regression of the neurological manifestations, cure and hospital discharge soon after the mastoidectomy and the drainage of the abscess. This fact was extremely gratifying for the whole team.
CONCLUSIONWe concluded that early diagnosis and approach of the primary infectious focus together with drainage of the abscess and appropriate antibiotic therapy is the right intervention to follow, aimed at reducing the rate of neurological sequelae and the length of hospital stay.
Isolated approach of trepanation or craniotomy presents high recurrence rates because the infectious focus remains in the contaminated middle ear.
The multidisciplinary team work should be a routine so that diagnosis and intervention may be conducted as early and effective as possible.
REFERENCES1. AYYAGARI, A.; PANCHOLI, V K.; KAK, U. K.; KUMAR, N.; KHOSLA, V K.; ARGAWAL, K. C.; GULATI, D. R. Bacteriological spectrum of brain abscess with special reference to anaerobic bacteria. Indian J. Med. Res., 77: 182-6, 1983.
2. BALLENGER, J. J. - Complicaciones de la otitis. In:_______- Enfermidades de la nariz, garganta, oido, cabeza y cuello. 3a ed. Barcelona, Salvate, 1988. pg.114166.
3. BRADLEY, E J.; MANNING, K. E; SHAW M. D. M. - Brain abscess secondary to otitis media. J. Laryngol. Otol., 98: 1185-91, 1984.
4. CAWTHORNE, T. - Discussion on diagnosis and treatment of cerebral abscess. Proc. R. Soc. Med., 38: 43840, 1945.
5. FERNÁNDEZ JULIAN, E.; SOLER, F.; SEGARRA, E Abscesso encefálico otogeno calcificado. An. ORL Ibero Am., 14: 305-10,1987.
6. GARFIELD, J. - Management of supratentoreal intracranial abscess: a review of 200 cases. Br. Med. J., 2: 2-11, 1969.
7. GOWER, D. & McGUIRT, W F. - Intracranial complications of acute and chronic infections ear disease: a problem still with us. Laryngoscope, 93: 1028-33, 1983.
8. GOYCOOLEA, M. V & JUNG, T. T K. - Complications of suppurative otitis media. In: PAPARELLA, M. M.; SHUMRICK, D. A.; GLUCKMAN, J. L.; MEYERHOFF, W L. - Otolaryngology. 3a ed. v II. Philadelphia, Saunders Company, 1991. pg. 1381-403.
9. HABIB, R. G.; GIRGIS, N. I.; ABU EL ELLA, A. H.; FARID, Z.; WOODY, J. -The treatment and outcome of intracranial infections of otogenic origin. J. Top. Med. Hug., 91: 836, 1988.
10. HARTER, D. H., - Parameningeal infections. In: WYNGAARTEN, J. B. & SMITH, H. H. - Cecil textbook of Medicine. Philadelphia, Saunders Company, 1985. pg. 2111-18.
11. KANGSANARAK, J.; FOOANANT, S.; RUCKPHAOPUNT, K.; NAVACHAROEN, N.; TEOTRAKUL, S. - Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J. Laryngol. Otol., 107: 999-1004, 1993.
12. KAPLAN, K. - Abscesso cerebral. In: MOLAWI, A.G. & LESROCK, J. L. - Clinica Medica da América do Norte. Interamericana, Rio de Janeiro, 1985. pg. 365-79
13. KARAMITSOS, D.; GAVALAS, G.; KARVELIS, N.; DOKIANAKIS, D. - Otogene hirnabzesse: neurochirurg oder otochirurg? HNO, 30: 60-2, 1982.
14. LEIBERMAN, A.; LUPU, L.; LANDSBERG, R.; FLISS, D. M. - Unusual complications of otitis media. Am. J. Otolaryngol., 15: 444-48, 1994.
15. MATHEWS, T. J.; MARUS, G. - Otogenic intradural complications: a review of 37 patients., Laryngol. Otol, 102: 121-4, 1988.
16. MORGAN, H.; WOOD, M. W.; MURPHEY, F. Experience with 88 consecutive case of brain abscess. J. Neurosurg., 38: 698-704, 1973.
17. PENIDO, N. O.; MOTA, E H.; MASCARI, D. S. A.; FUKUDA, Y - Abscesso cerebral de origem otogenica. Relato de um caso. Acta Awho, 9: 32-5, 1990.
18. PENIDO, N. O. - Abscesso encefálico otogênico: tratamento a evolução. São Paulo, 1992. Tese de Mestrado, Escola Paulista de Medicina.
19. PROCTOR, C. A. - Intracranial complications of otitis origin. Laryngoscope, 76: 288-308, 1966.
20. QUIJANO, M.; SCHUKNECHT, H. F.; OTTE, J. Temporal bone pathology associated with intracranial abscess. ORL, 50: 2-31, 1988.
21. ROSENBLUM, M. L.; HOFF, J. T.; NORMAN, N.; WEINSTEIN, E R.; PITTS, L. - Decreased mortality from brain abscess since advent of computed tomography. J. Neurosurg., 49: 658-68, 1978.
22. VINCENT, C. - Le traitement des abces subaigus et chroniques des hemisphere. Men. Acad. Chir, 64: 661-73, 1938.
23. WRIGHT, J. L. W & GRIMALDI, E M. G. B. - Otogenic intracranial complications. J. Laryngol. Otol., 87:1085-96, 1973.
24. WHELAN, M. A. & HILAL, S. K. - Computed tomography as a guide in the diagnosis and follow-up of brain abscess. Radiology, 135: 663-71, 1980.
* Ph.D. in Medicine - Universidade Federal de São Paulo - Escola Paulista de Medicina (UNIFESP-EPM).
** Full Professor - UNIFESP - EPM.
Address correspondence to: Norma de Oliveira Penido - Universidade Federal de São Paulo - Escola Paulista de Medicina.
Rua Botucatu, 740 - 3° Andar - 04023-901 São Paulo/SP.
Article submitted on December 18. 2000. Article accented on February 8, 2001.


