INTRODUCTIONIn 1880, Graefe described a child with inexpressive face, representing the first description of Moebius sequence13. From then on, other similar cases were reported, and the main clinical characteristics were: bilateral facial paralysis, converging strabismus, tongue and masseter atrophy, micrognatia, equinovarus, syndactyly and arthrogryposis. Other less frequent manifestations are soft palate paralysis, deafness, mental retardation (in less than 15 % of the cases), cleft palate, dextrocardia and ventricular septum defects5,6,7.
Although etiology of Moebius sequence has not been defined yet, drug induction has played a key role, based on the frequent reports of mother who claimed they had used misoprostol in the early stages of pregnancy. It is a drug that belongs to prostaglandin E1 category, marketed as Cytotec®, which is originally indicated for the treatment of gastric and duodenal ulcer. One of the side effects of the drug is uterine contractions and vaginal hemorrhage, responsible for many cases of abortion; from that fact stems the illegal use of the drug to provoke abortion of an undesirable pregnancy5,13,14. However, if the abortion fails, the pregnancy proceeds with the effects of the medication on the fetal development.
The ENT repercussions of Moebius sequence, secondary to cranial nerve paralysis, involve key motor and sensorial functions, such as suction, mastication, facial mimics, articulation and hearing, requiring a multidisciplinary approach for diagnosis and management.
Owing to the constellation of clinical manifestations and the variable expressions of Moebius sequence, we decided to carry out a study with such patients to record the main physical alterations and the consequent functional limitations, in addition to hearing acuity and detection of possible etiological factors.
MATERIAL AND METHODThe studied group consisted of 5 Moebius sequence children, aged from one year and twelve months to twelve years, seen at the Ambulatory of Otorhinolaryngology and Head and Neck Surgery at Faculdade de Medicina de Botucatu (Unesp). After approval of the protocol by the Ethics Committee and the signature of the informed consent by the parents, children were submitted to complete general and ENT physical examinations, including hearing tests. All the children had been submitted to genetic evaluation to confirm diagnosis.
Based on data provided by the medical files and interviews with the parents, we collected data concerning the potential etiological factors involved in the development of congenital anomalies.
In the hearing assessment, children under the age of two years were submitted to behavioral tests with calibrated noisemakers. Children over 2 years were tested with pure tone conditioned or conventional audiometry (audiometer Madsen OB822), depending on the level of understanding and the reliability of responses. All children were submitted to immitanciometry (Amplaid 75) and auditory brainstem evoked potential (ABR). ABR was carried out with the device brand Nihon Koden (MEB 7102 k). Positive electrodes were fixed on the forehead and negative electrodes were fixed on retroauricular regions, after scrubbing with alcohol and abrasive substance. The grounding electrode was placed on the wrist. Stimulation was monoaural, at 85 dB, with 40 dB contralateral masking. We used 2,000 sweeps, duration of 10 ms, repeated by confirmation or reproducibility of waves. The intensity of stimulus was increased up to 100 dB if there were no recordings at 85 dB.
RESULTSThere were three male and two female patients, aged 1y2m to 12 years. The use of misoprostol at early pregnancy stages were reported by four mothers and ignored by one.
Table 1 lists the most marked alterations, observed in the physical examination of all evaluated children: bilateral facial paralysis, unilateral masseter atrophy, dental malocclusion, retraction and/or thickness of tympanic membrane, equinovarus, oblique palpebral fissure and tongue atrophy. Other less frequent alterations were micrognatia, converging strabismus, soft palate paralysis, syndactyly and low implantation of ears.
Table 2 summarizes the results of otoscopy and hearing assessment. Otoscopy was altered in all children, with variable degrees of retraction and/or thickness of tympanic membrane. Signs of auditory tube obstruction were evidenced by tympanometry, through curves C or B, present in all children. Audiometric tests revealed conductive hearing loss in three children and mixed hearing loss in one case (Case 4), who presented a significant degree of tympanic membrane retraction. Behavioral tests with noise-makers were used in only one child, aged 1 year and 2 months (case 1), who responded correctly to all stimuli.
In Figures 1, 2 and 3 we presented the results of auditory brainstem evoked potentials of patients who presented abnormal responses (ABR I, II and III, respectively). In Figure 1, we may notice that electrophysiological potentials on the left were present at 85 dB, with normal values for absolute wave latency (P-I, RIII; P-V) and interpeak latency (LIP). On the right, we observed prolonged absolute wave latency, as from PI, and the same interpeak latency (LIPS: I-III, III-V I-V), alterations detected in the cases of conductive hearing loss. Similar recordings are presented in Figure 2. In Figure 3 we observed that electrophysiological potentials were absent at 100 dB on the right. On the left, at 100 dB, it was possible to identify the recordings of electrophysiological potentials with values within normal ranges. These alterations are typical of sensorineural or mixed hearing losses.
TABLE 1 - Main clinical manifestation in children with Moebius syndrome.
TABLE II - List of evaluated children and respective ages. Results of otoscopy and hearing acuity tests.
In Moebius sequence, the impairment of cranial nerves VI and VII is detected at birth because of the inexpressive face, opened palpebral fissure during sleep, difficulty to suck and converging strabismus. Alterations of oral motor system are more affected if associated with tongue and masseter atrophy, by the involvement of V and XII cranial nerves, and micrognatia6,8,10. Owing to these factors, these children present alterations of mastication pattern, especially during the oral phase. The food is cut only on one side of the dental arch and remains a long time against the internal face of the cheeks, in constant contact with the teeth, compromising oral hygiene and predisposing to caries. Intraoral proprioception is poor, normally generating constant sialorrhea. These children remain with their mouths opened, they have incompetent lip sealing and hypotonic and retracted lips (Figures 4 and 5). The lack of sustention of masseter, associated with the previously described factors, is responsible for dental malocclusion, presented in all children studied in the present report.
Figure 1. Right ear, prolonged isolated wave latency (P-I, P-III, P-V), and normal values of interpeak latency (LIPS: I-III, III-V; I-V). Left ear - normal ABR.
Figure 2. Right ear - normal ABR. Left ear - prolonged isolated wave latency (P-I, P-III, P-V), and normal values of interpeak latency (LIPS: I-III, III-V; I-V).
Limb impairment varies from severe malformations, such as arthrogryposis and total agenesis of hands and feet, to finger abnormalities (syndactyly) and joint deficit (equinovarus). The latter was a constant finding of the physical examination of the studied children (Figures 6a, 6b and 7), confirming the description of other authors5,6,8,10.
Cognitive aspects are less affected and intellectual retardation is present in only 10 to 15% of the cases9. However, owing to physical limitations and communication difficulties, they present poor school and social-emotional performance.
As to language, receptive is better than expressive language. Articulation is impaired, especially in the production of bilabial phonemes, which depend on lip sealing. Articulation is imprecise, poor and restricted to the movement of atrophic tongue against the articulation points. If there is paralysis of soft palate muscle, which may be associated with the condition, as observed in one of the subjects, voice production may be hypernasal, hindering understanding.
Figure 3. Right ear - absence of response at 100 dB. Left ear - normal ABR at 100 dB.
Communication is also affected by the onset of varied degree hearing loss, present in four of the five children. Conductive hearing loss is more common, owing to predisposing factors, such as, perioral muscle hypotonia, complementary mouth breathing and possible paralysis of soft palate muscles, which are important in the physiological mechanism of auditory tube contraction and middle ear pressure control. These factors justify the abnormal results of otoscopy and tympanometry in all studied children.
As a result of aging and thanks to the support of the physical and speech, therapists adaptation and compensation mechanisms of the non-affected muscles are activated, such as improvement of palpebral occlusion, better mastication control, salivation and swallowing. On the other hand, otological sequelae seem to be inevitable and in the first years of life we may observe alterations in otoscopy, even without the detection of hearing loss, as observed in one of the subjects (case 1), in which responses to noise-makers and ABR were within normal ranges, whereas otoscopy was altered and showed slight retraction and thickness of the tympanic membrane, showing type C tympanometric curve.
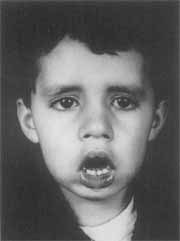
Figure 4. Child with Moebius sequence (case 1). Inexpressive face, converging strabismus, lip hypotonia and micrognatia.
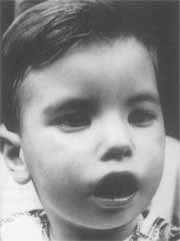
Figure 5. Child with Moebius sequence (case 2). Inexpressive face and marked sialorrhea.


Figure 6a and 6b. Hand malformation (syndactyly) in children with Moebius sequence.
As the age increases, the patients may experience aggravation of the auditory tube obstruction and severe retraction of tympanic membranes, which may become adhered to the middle ear, characterizing cases of adhesive otitis media. They may be associated with mixed hearing loss, because of rigidity of ossicle chain and ototoxic action of chemical mediators released in the chronic inflammatory process3,4. These data explain the severe degree of hearing loss detected in case 4, who presented adhesive otitis media on the right, type B tympanometric curve and absence of responses at 100 dB in the ABR on the same side.

Figure 7. Feet malformation (equinovarus) in children with Moebius sequence.
The involvement of the VIII cranial nerve in this pathology is not frequent and it was not observed in the present study6.
As to possible etiological agents related to Moebius sequence, the use of misoprostol (Citotec®) in the first trimester of pregnancy was reported by four mothers and not excluded by one adopted mother, since she knew of the attempts of the natural mother to have an abortion. The literature brings some studies that suggest such a relation; however, the exact pathophysiology of the action mechanism of these drugs on the physical alterations observed in Moebius sequence has not been fully determined yet1,5,6,11,12,13,14,15. It is believed that the uterine contractions caused by misoprostol during the first weeks of life, when the amount of amniotic fluid is quite low, lead to exaggerated cervical flexion of the fetus, which may press the nuclei of cranial nerves VI and VII; because of the proximity of the location in the embryo, it results in local ischemia and agenesis or atrophy of the nervous structures at the level of the nuclei of the corresponding cranial nerves13,14. Degree and site of ischemia may explain the involvement of other cranial nerves in Moebius sequence, as well as the phenotype alterations observed in patients. Other hypotheses for the action mechanism of the drug are vascular collapse, brainstem ischemia, nuclear aplasia, and primary neuromuscular' disease7,10,15,16.
Autopsy of newborns with Moebius sequence, in which the mother had reported use of misoprostol during pregnancy, revealed agenesis of cranial nerves VI, VII and VIII, ventricular dilation, poorly marked thalamic nuclei, demyelinated and poorly oriented axons, calcification of cranial nerve nuclei and focal necrosis15,16. Similar alterations were described after the use of benzodiazepine during gestation2. Therefore, there are strong indications of the drug induced genesis of Moebius sequence.
CONCLUSIONIn the present study, cranial nerves affected in children with Moebius sequence were V VII and XII, responsible for motor and sensorial key regions of the body. Although it is a congenital abnormality, new clinical manifestations may result from maturation, such as hearing loss, poor school performance, communication and social-economic disorders, secondary to primary structural alterations. The use of misoprostol in the early stages of pregnancy was a frequent report, indicating that it might be an important etiological factor.
REFERENCES1. COSTA, S. H.; VESSEY, M. E - Misoprostol and illegal abortion in Rio de Janeiro. Lancet, 341: 1256-61, 1993.
2. COURTENS, W; HAINAUT, M. - Moebius syndrome in an infant exposed in uterus to benzodiazepines. J. Pediatrics, 121: 833-34, 1992.
3. DUBREUIL, C. - Otite seromuqueuse. JFORL, 45: 3944, 1996.
4. GLODDEK, B.; LAMM, K. E.; HASLOV K. - Influence of middle ear immune response on the immunological state and function of the inner ear. Laryngoscope, 102:117-118, 1992.
5. GONZALEZ, C. H.; VARGAS, F. R.; PEREZ, A. B. A; KIM, C. A.; BRUONI, D.; DIAS, M. J. A.; LEONE, C. R; CORREA, J. NETO.; LLERENA, J. C. Jr.; ALMEIDA, J. C. C. - Limb deficiency with or without Mobius sequence in seven Brazilian children associated with misoprostol use in the first trimester of pregnancy. Am. J Med. Genetics, 47: 59-64, 1993.
6. GONZALEZ, C. H.; DIAS, M. J. M.; KIM, C. A.; SUGAYAMA, S. M. M.; PAZ, J. A.; HUSON, S. M.; HOLMES, L. B. - Congenital abnormalities in Brazilian children associated with misoprostol misuse in first trimester of pregnancy. Lancet, 351: 1624-27, 1998.
7. GOVAERT, T. E; VANHAESEBROUCK, E; PARETER, C.; FRÄNKEL, U.; LEROY, J.; - Moebius sequence and prenatal brainstem ischemia. Pediatrics, 84: 570-73, 1989.
8. HASLAM, R. H. A.; LOWRY, R. B. - In: BUYSE, M. L. Birth Defects Encyclopedia, 1st ed., Dover, Center for Birth Defects Information Service, 1990, 542-543.
9. JARADEH, S.; D'CRUZ, O.; HOWARD, J.; HABERKAMP, T; KONKOL, R.; -Möbius syndrome: eletrophisiologic studies in seven cases. Muscle & Nerve, 19: 1148-53, 1996.
10. MUSTACCHI, Z. - In: MUSTACCHI, Z.; PEREZ, S. Genética Baseada em Evidências: Síndromes a Heranças, 1ª ed., São Paulo, Cid Editora, 2000, 1105-1110.
11. NORMAN, J. E.; THONG, K. J.; BAIRD, D. T -Uterine contractility and induction of abortion in early pregnancy by misoprostol and mifepristone. Lancet, 338: 1233-36, 1991.
12. PASTUSZAK, A. L.; SCHULLER, K. A.; COELHO, F.; VARGAS, D.; MARTINS, S. - Misoprostol use during pregnancy is associated with a increased risk for Moebius sequence. Teratology, 51:36, 1989.
13. PITNER, S. E.; EDWARDS, J. E.; McCORMICK, W F. Observations on the pathology of the Moebius syndrome. J. Neurol. Neurosurg. Psychiatry, 28: 362-67, 1965.
14. SHEPARD, T. H. - M6bius syndrome after misoprostol: a possible teratogenic mechanism. Lancet, 346: 780, 1995.
15. SCHÖNHÖFER, E S. - Brazil: misuse of misoprostol as an abortifacient may induce malformations. Lancet, 337: 1534-35, 1991.
16. THAKKAR, N.; O'NEIL, W; DUVALLY, J.; LIU, C.; AMBLER, M.; - Möbius syndrome due to brainstem tegmental necrosis. Arch. Neurol., 34:124-26, 1977.
* Assistant Professor, Ph.D., Discipline of Otorhinolaryngology and Head and Neck Surgery, Faculdade de Medicina de Botucatu - UNESP
** Resident, Discipline of Otorhinolaryngology and Head and Neck Surgery, Faculdade de Medicina de Botucatu - UNESP
*** Speech and Hearing Pathologist, Discipline of Otorhinolaryngology and Head and Neck Surgery, Faculdade de Medicina de Botucatu - UNESP
Study conducted at the Discipline of Otorhinolaryngology and Head and Neck Surgery, Faculdade de Medicina de Botucatu - Department of Ophthalmology,
Otorhinolaryngology and Head and Neck Surgery - UNESP- São Paulo.
Study presented at 35° Congresso Brasileiro de Otorrinolaringologia, held on October 18, 2000, in Natal /RN.
Address correspondence to: Regina Helena Garcia Martins - Departamento de Oftalmologia, Otorrinolaringologia a Cirurgia de Cabeça a Pescoço - Faculdade de Medicina de Botucatu - UNESP - 18618-000 Botucatu /SP - Tel/Fax: (55 14) 6802-6256 - E-mail: rmartins@fmb.unesp.br
Article submitted on November 13, 2000. Article accepted on March 1, 2001.


