INTRODUCTIONTumors (or masses) originated from the nasal fossa may be benign or malignant. Inflammatory nasal polyps, for example, may be unilateral or bilateral. Unilateral lesions most commonly found are antrochoanal polyps, encephalocele, inverted papilloma, angiofibroma, carcinoma and sarcoma, among other affections3.
As we can observe, differential diagnosis is necessary because of the different therapeutic interventions recommended for each case. If a patient has unilateral nasal obstruction, we should concentrate on pathologies that initially present this symptom.
In the case reported below, the initial diagnosis of antrochoanal polyp was made (anamnesis and physical exam). During paranasal cavity CT scan, we noticed the involvement of soft parts and the bone of the inferior turbinate on the right nasal fossa, characterizing a fibro-osseous lesion restricted to the inferior turbinate. Owing to the rarity of this affection in the region, we performed a review of the literature and reported the case that follows.
REVIEW OF LITERATUREA large variety of lesions may involve maxillofacial bones7. Ossifying fibroma and fibrous dysplasia are the most common types of fibro-osseous lesions that affect craniofacial bones1. Despite the differences in clinical and radiological manifestations, the commonality between these two lesions is the replacement of the normal bone architecture by benign fibrous tissue, which contains a variable quantity of mineralized material1. The identification of a fibro-osseous lesion depends on the history of the patient, clinical findings, radiological criteria and histopathological analysis1.
There is no agreement when it comes to the classification of fibrous-osseous lesions. An objective classification, described by Waldron (1983) and Kramer et al. (1992), and quoted by Slootweg (1996)7, classified the lesions into: fibrous dysplasia (polyostotic and monostotic); ossifying fibroma (conventional, psamomatoid and juvenile), and periapical cemento-dysplasia. Brademann et al (1997)4 mentioned another aggressive form, locally destructive and with high rate of ossifying fibroma recurrence, which is the so-called cemento-ossifying fibroma, whose lesion was reported on the petromastoid region, published in the literature for the first time. As to fibrous dysplasia, a third clinical form that has not been cited by the author is the disseminated form, also called McCune-Albright syndrome with systemic manifestations6. Ossifying fibroma, as reported, is a commonly detected lesion on the facial bones, especially on the mandible (maxillary sinus involvement is not common), responsible for 75% of the cases2. However, giant lesions (larger than 8cm) are most commonly found in the maxilla2. Ossifying tumors may surge at any age range, but the mean age of affected subjects is 31 years2. It is more common in women, with women: men ratio of 1.6:1. Since they axe benign lesions with no deformity, curettage and osteotomy may be enough to treat them, producing recurrence rates that vary from 0% to 28%2. Ossifying fibromas share some histopathological characteristics with another type of fibroosseous lesion called fibrous dysplasia. In addition, the lesion sometimes looks like a well-differentiated osteosarcoma, especially in histologic forms that present increased cellularity and number of mitosis7.
CASE REPORTM. S. M, female 68 year-old married patient, born in Minas Gerais and currently a housewife in Rio de Janeiro.
Main complaint: nasal obstruction on the right
Personal history: Patient referred that one year and half ago she started to feel insidious and progressive right nasal obstruction. She did not have headache, rhinorrhea, epistaxis, nasal discharge or sneezing episodes. She experienced improvement in breathing when she started treatment with injecting betamethasone and nasal spray beclomethasone dipropionate.
Previous pathologies: Controlled high blood pressure and hypercholesterolemia.
She did not report use of alcohol or smoking.
ENT exam: oroscopy - no alterations. Anterior rhinoscopy - lesion similar to a nasal polyp occupying the right nasal fossa. Left nasal fossa with no alteration. Otoscopy - no alterations.
CT Scan: material with soft part density occupying the right nasal fossa. Concentric mucosa thickness on the right maxillary sinus (floor). Inside the mass, there was destruction of the inferior turbinate bone. Spotted lesion, no invasion into adjacent structures (Figures 1 and 2).
Nasal endoscopy: Firm consistent polyp occupying the right nasal fossa, obstructing the middle meatus. The inferior turbinate was not differentiated from the rest of the lesion. No further alterations.
The patient was submitted to surgery for the removal of mass. During the surgery, we noticed that the mass corresponded to a large degeneration of the anterior and middle portions of the inferior turbinate. Middle meatus and turbinate were intact. The whole lesion was removed en bloc (Figure 3 and 4).
Evolution: the patient progressed satisfactorily, restoring right nasal fossa breathing. She remains asymptomatic 15 months after the surgery.

Figure 1. CT, at axial section showing a lesion occupying the right nasal fossa. Note the bone destruction involving the inferior

Figure 2. CT, at coronal section. Spotted bone lesions involving the bone of the inferior turbinate.

Figure 3. Surgical piece, external face. Polypoid lesion corresponds to the anterior third of the inferior turbinate.

Figure 4. Surgical piece, internal face. The posterior third of the inferior turbinate is preserved.
Histopathologlcal report:
Macroscopy: lesion similar to a polyp with pedicle, distal extremity is rounded, of elastic consistency, glossy external surface and section surface of mixoid aspect. The three proximal quarters have firm consistency, light brown color and ossified areas in the center.
Microscopy: edema and marked congestion of mucosa throughout the whole mass. The areas of bone proliferation present new trabeculae formed by lamellar deposit from the matrix, involved by countless osteoblasts. The adjacent stroma has fibrous, mixoid and hypocellular aspect. Such characteristics define the diagnosis of ossifying fibroma (Figures 5 and 6).
DISCUSSIONAt first sight, data from the anamnesis and physical exam suggested antrochoanal polyp, which was the first hypothesis made.
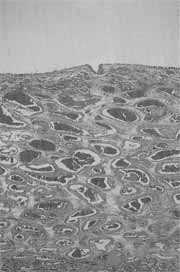
Figure 5. Intense edema and congestion of respiratory mucosa of inferior turbinate (H&E, 40x).

Figure 6. Neoformation of bone trabeculae involved by osteoblasts and fibrous tissue (H&E, 40x).
However, paranasal sinuses CT scan helped identify a lesion that compromised the inferior turbinate bone, without obstructing the ostium-meatal complex, which in most cases is impaired both in antrochoanal polyps and in nasal polyposis. The lesion was circumscribed and had well defined margins with no invasion of subjacent bone areas. Upon the confirmation of bone diagnosis, we conducted differential diagnosis with fibrous dysplasia and sarcoma. Fibrous dysplasia, ossifying fibroma and cemento-ossifying fibroma are lesions with osseous and fibrous components that share some histopathologic characteristics, but there are details important for differentiation. In the case of fibrous dysplasia, bone trabeculae involved in the fibrous tissue normally merge with the surrounding bone, presented irregular branches and absence of osteoblasts on the margins of the trabecula5. On the other hand, in ossifying fibroma we normally find lamellar bone well marked with osteoblasts. The trabeculae tend to be more continuous'. Ossifying fibroma is characterized by different histologic appearance, that is, the fibrous tissue may vary considerably in the same lesion, with areas of high cellularity alternated with more collagen or sclerotic portions7. The fusion of trabecular bone may result in large bone "islets" that form most of the lesion.
In an attempt to reach the correct diagnosis, Boysen et al. (1979), cited by Sternberg (1994)5, stated that "the differential diagnosis between fibrous dysplasia and ossifying fibroma depends on radiological criteria once the pathologist has identified the fibrous-osseous nature of the lesion". Differently from the fibrous dysplasia, ossifying fibroma is an expansive and well delimited lesion, although opacity of the lesion varies according to its maturity. The most marked characteristic of fibrous dysplasia in CT scan is the appearance of "translucent glass", in addition to poorly defined margins.
FINAL COMMENTSMaxillofacial fibro-osseous lesions continue to be a diagnostic quandary both for the clinician and the pathologist. Owing to uncertainties concerning specificity of clinical, radiological and histopathological diagnoses, there is no classification that is completely satisfying or acceptable for these lesions. The only point of agreement is that it requires multidisciplinary approach, involving experienced otorhinolaryngologists, radiologists and pathologists in order to define the prognosis of the pathology and the correct treatment.
REFERENCES1. BEASLEY, D. J.; LEJEUNE, F. E.- Fibro-osseous lesions of the head and neck] La. State Med. Soc., 148: 413-415, 1996.
2. CHONG, V F. H; TAN, L. H. C. - Maxillary Sinus ossifying fibroma. Am. J. Otolaryngol., 18(6): 419-424, 1997.
3. FELDMAN, B. A.; FELDMAN, D. E. - In LEE, K. J. - Essential Otolaryngology Head & Neck Surgery, 6th ed., Connecticut, Appleton & Lange, 1995, 715-756.
4. BRADEMANN, G; WERNER, J; JANIG, U; MEHDORN, H. M.; RUDERT, H. - Cemento-ossifying fibroma of the petromastoid region: case report and review of the literature. J. Laryngol. Otot, 111: 152-155, 1997.
5. MILLS, S. E.; FECHNER, R. E.- In STERNBERG, S. S. et al. - Diagnostic Surgical Pathology, 2nd ed., New York, Raven Press, 1994, 851-891.
6. SANCHEZ, J. C.; CABALLERO, D. H. B.; CALATAYUD, M. F. R. - Displasia fibrosa monostótica de maxilar superior. Presentación de un caso clínico. Acta Otorrinolaringol Esp., 48(7): 579-582, 1997.
7. SLOOTWEG, E J. - Maxillofacial Fibro-osseous Lesions: Classification and Differential, Diagnosis. Semin. Diagn. Pathol., 13(2): 104-112, 1996.
* Master studies in otorhinolaryngology under course, Faculdade de Medicina da Universidade Federal do Rio de Janeiro (UFRJ).
** Physician and Preceptor of Medical Residence, Service of Otorhinolaryngology, Hospital Universitário Clementino Fraga Filho (HUCFF), UFRJ.
*** Joint Professor of the Discipline of Otorhinolaryngology Faculdade de Medicina da UFRJ.
**** Assistant Professor and Head of the Service of Otorhinolaryngology, HUCFF.
***** Assistant Professor, Department of Pathology, Faculdade de Medicina da UFRJ.
Study conducted at Service of Otorhinolaryngology, Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro.
Address correspondence to: Dra. Carla Ribeiro Monteiro - Rua Alceu Amoroso Lima 105/901 - Barra da Tijuca - 22631-010 Rio de Jateiro /RJ. Tel: (55 21) 9626.2987
Fax: (55 21) 430.9120 - E-mail: comcarla@openlink.com.br
Article submitted on August 4, 2000. Article accepted on September 14, 2000.


