INTRODUCTIONThere are countless causes and characteristics of traumatic lesions of the oral mucosa. A topic frequently addressed by articles, authors are unanimous to say that clinical characteristics of oral lesions may be very similar, regardless of the etiology (traumatic lesion, benign tumor or initial phase malignant tumor). Therefore, pathology and anamnesis are essential to confirm the diagnosis.
Acute traumas are normally deeper lesions and they may progress to hematoma, erosions or ulcers. Agents vary a lot and episodes are on purpose or by accident2. When chronic, there is normally increase in connective tissue, growing around the initial lesion. The traumatic agent may also determine continuous or repetitive lesions.
The most common sites for this kind of lesions are the tip of. the tongue, palate, lips and jugal mucosa, normally affected by fibrous hyperplasia, papilla hyperplasia, morsicatio buccarum et labiorum, epulis fissuratum, mucous cysts and many others.
There are few references about the topic, especially in the Brazilian literature. Based on the above, the present study intended to evaluate different oral mucosa affections by traumatic etiology, treated at the Ambulatory of Stomatology of Santa Casa de Misericórdia de São Paulo, presenting prevalence according to gender, age, site, traumatic agent and type of lesion.
MATERIAL AND METHODSixty-seven cases of oral mucosa traumatic lesions (between 1997 and 2000) were retrospectively assessed in the Ambulatory of Stomatology of the Department of Otorhinolaryngology at Santa Casa de Misericórdia de São Paulo (SCMSP).
Diagnoses were based on clinical history and pathology of lesions. Biopsies were conducted at the Operating Room of the Department of Otorhinolaryngology at the institution, under local anesthesia. Histologic analyses were conducted by the Department of Anatomic Pathology.
We collected data concerning gender, age, affected site, etiology and type of lesion from the admission files of patients at the, Ambulatory of Stomatology.
RESULTSIn the present study, we analyzed 67 lesions found in 65 patients. Among them 40 (61.5%) were female patients and 25 (38.5%) were male patients. Ages ranged from 4 to 82 years, but most of the cases were concentrated between the fourth and the seventh decades of life (64.7%). Two cases were of children below 10 years of age and three subjects were older than 81 years. Distribution of patients according to gender and age is illustrated in Graph 1.
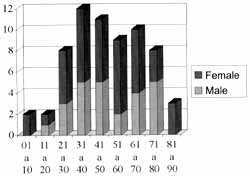
Graph 1. Distribution of age and gender.
By characterizing the different etiological agents causing traumatic lesions we listed dental prostheses, bites, missing teeth and chemical cauterization of mucosa. Dental prostheses and bites were the key elements responsible for oral mucosa lesions of patients in the ambulatory. Together, they accounted for 95.4% of the cases: the former was responsible for damage in 25 patients (38.5%), whereas the latter accounted for 37 (56.9%). Missing teeth were the cause of oral mucosa affection in only two cases (3.07%), both men, and cauterization caused it in one 47year-old woman (1.53%). In the case of prostheses, 18 patients were female (72%) and seven were male (28%). As for bites, the female prevalence was also noticed, but at a lower proportion: 16 men (43.25%) to 21 women (56.75%). Graph 2 clearly shows the correlations.
As to site of lesions, we detected lips, tongue, gingival-fugal region, palate and floor of the mouth. In Graph 3 we can see that the tongue was affected in 29 (43.28%) of the cases, followed by gingival and jugal mucosa (19 patients - 28.36%). Only seven cases (10.45%) had lip lesions, as opposed to nine (34.43%) in the palate and three (4.48%) in the floor of the mouth. Regardless of the site, the incidence in women was higher, except for the floor of the mouth, which was a site only affected in men.
Upon macro and microscopic analysis of lesions, we observed that fibrous hyperplasia (Figure 1) was the most frequent manifestation of oral mucosa traumatic lesions in the Ambulatory. It accounted for 28 cases (41.79%), affecting especially women, at a proportion of four women to one man (22 women and 6 men), mainly distributed between the 4th and 7th decades of life. Hyperplasia of foliate papilla was responsible for 5 cases (7.47%) and hemangioma and leukoplasia had four cases each (5.97%). There was one case of aphtha, one case of Stenon's duct edema, one case of deepithelization and two cases (2.98%) of mucous cyst (Figure 2). The remaining patients presented lesions which were not fully diagnosed by the pathology: there were nine ulceration, eight hyperemia cases, one ecchymosis, one vegetating lesion, one thick and one elevated lesions. Table 1 shows the distribution of these lesions according to gender and Table 2 illustrates the distribution of lesions based on affected site and traumatic agent.
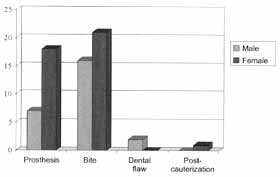
Graph 2. Distribution of traumatic agents by gender.
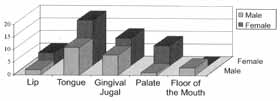
Graph 3. Distribution of lesion site by genger.

Figure 1. Gingival-jugal fibrous hyperplasia.

Figure 2. Lip mucous cyst.
TABLE 1 - Distribution according to gender.
Table 2 - Distribution of lesions according to affected site and agent of trauma.
Most of mouth infections are a response of the tissue to a non-specific infection, irritation factor and/or trauma. These aggression factors promote the proliferation of epithelial and inflammatory cells, fibroblasts, collagen and blood vessels, which may lead to tissue destruction. According to the specific cause, we may clinically classify lesions based on: a) presence or absence of ulceration; b) consistency; c) color; d) with pedicle or sessile, and e) associated or not with destruction and bone neoformation. Histologically, the variations are: a) degree of vascular proliferation; b) inflammatory process; c) excess of collagen; d) giant cells, and e) osteoclastic and osteoblastic activity1. Based on these criteria, it is possible to diagnose and classify the lesions in order to facilitate management.
With this in mind, Anneroth and Sigurdson, 1983, proposed the following classification:
• Granulomatous lesions: they have a significant inflammatory process, in addition to intense vascular proliferation. The epithelium is normally thin, with ulceration and recovered by fibrin. There are countless polimorphonuclear cells, with immature fibroblasts and some giant cells. There is prevalence in female patients (maybe because of hormones) and the main examples are pregnancy tumors, pyogenic granuloma and epulis angiomatosum.
• Fibromatous lesions: rich in collagen, they present discreet inflammatory process and poor vascular supply. In addition to achantosis, hyperkeratosis and absence of giant cells, there may be metaplastic bone proliferation. Although Cutright said in 1974 that they were more prevalent in women (for esthetical purposes, women use dental prostheses longer), the other studies showed that there are no gender differences, but a higher prevalence between the fourth and fifth decades of life1,7. The main examples are fibrous hyperplasia and epulis fissuratum. It is important to highlight that the classic term fibroma is incorrectly used, because the word involves the specific concept of benign tumor of connective tissue by proliferation of fibroblasts and should be submitted to differential diagnosis with neurofibroma, leiomyoma and angioleiomyoma3.
• Giant cell lesions: abundant giant cells, especially osteoclastic cells, in the embryonictype mesenchymal stroma (primitive), with the presence of fibroblast, high osteoclastic action and low level inflammatory process. The presence of hemosiderin is normally observed and the lesion is recovered by a multi-layered epithelium restricted to the gums and the alveolar process. Owing to the intense osteolytic action, the degree of alveolar destruction is very prevalent in the lesion, requiring larger resection margins, including the periosteum and, sometimes, the superficial bone layer.
In the present study we did not detect giant cell lesions, but fibromatous lesions were the most predominant in 41.79% of the cases. Although there was no direct correlation between fibrous hyperplasia and female genders, our study produced data similar to the ones reported by Cutright in 1974, with an incidence of 78.57% women cases. One possible explanation is that since women are more beauty-conscious, they wear dental prostheses longer.
One very common affection according to the literature, the morsicatio buccarum et labiorum5,6,8,9,10, which despite the pathognomonic histology is frequently misdiagnosed, was not detected among our cases. It starts from a simple whitish lesion and may progress to lip or jugal mucosa erosion. Caused by the continuous habit of biting the lips, it has psychogenic correlation11 and should not be forgotten by clinicians and pathologists.
It is important to point out that in our sample lesions caused by poorly adapted dental prostheses and bites were predominant, probably because of unresolved occlusion problems and poor conditions of dental conservation. Such data reflect the poor dental conditions of our population, as well as the difficulty to access basic dental care, which is even more significant for orthodontic treatment due to the low social-economic level of the population.
Needless to say, not all lesions are symptomatic and they may be overlooked by the patient and the physician. In our opinion, it could be a reason for the statistical discrepancies with the literature.
In summary, oral mucosa traumatic lesions are very prevalent in the Brazilian population and reflect poor dental conditions.
Appropriate diagnosis is important not only to prevent recurrence and repetitive surgical procedures, but also progression of the lesion and, occasionally, malignant transformation. Patients should be referred to oral rehabilitation (prosthesis fitting, dental treatment, correction of occlusal problems) and, if necessary, psychological follow-up in case of continuous bites.
REFERENCES1. ANNEROTH, G.; SIGURDSON, A. - Hyperplastic lesions of the gingival and alveolar mucosa. Acta. Odontol Scand., 41 (2): 75-86, 1983.
2. BORK, K.; HOEDE, N.; KORTING, G. W; BURGDORF, W H.; YOUNG, S. K. - Diseases of the Oral Mucosa and the Lips. English edition, 1996.
3. CHRISTOPOULOS, P; SKIAVOUNOU, A.; PATRIKIOU, A. - True fibroma of the oral mucosa: a case report. Int. J. Oral. Maxillofac. Surg., 23: 98-99, 1994.
4. CUTRIGHT, D. E. - The histopathologic findings in 583 cases of epulis fissuratum. Oral. Surg. Oral. Med. Oral. Pathol., 37(3): 401-411, 1974.
5. GLASS, F.; MAIZE, J. C. - Morsicatio Buccarum et Laborium (Excessive Cheek and Lip Biting). Am. J. Dermatopathol, 13:271-274, 1991.
6. HATJIGIORGIS, C. G.; MARTIN, J. W - An interim prosthesis to prevent lip and cheek biting. J. Prosthet Dent., 59 (2): 250-252, 1988.
7. HOUSTON, G. D.; BROWN, F. H. - Differential Diagnosis of the Palatal Mass. Compendium., 14 (10): 1222-1232, 1993.
8. Letter: Leukodema, reactive hyperkeratosis, or cheek biting. Arch. Dermatol., 117 (8): 454-455, 1981.
9. SCHIODT, M.; LARSEN, V; BESSERMANN, M. - Oral findings in glassblowers. Community. Dent. Oral Epidemiol; 8 (4): 195-200, 1980.
10. SINGH, T -An appliance for the management of cheek biting. J. Indian. Dent. Assoc., 43: 18-19, 1971.
11. WALKER, R. S.; ROGERS, W A. - Modified maxillary occlusal splint for prevention of cheek biting: A clinical report. 1. Prosthet Dent. 67- 581-582, 1992.
* Master studies under course, Department of Otorhinolaryngology, Faculdade de Ciências Médicas, Santa Casa de Misericórdia de São Paulo.
** Doctorate studies under course, Department of Otorhinolaryngology, Faculdade de Ciências Médicas, Santa Casa de Misericórdia de São Paulo.
*** Joint Professor, Department of Otorhinolaryngology, Faculdade de Ciências Médicas, Santa Casa de Misericórdia de São Paulo.
Address correspondence to: Faculdade de Ciências Medicas da Santa Casa de São Paulo - Departamento de Otorrinolaringologia - Rua Cesário Motta Junior, 61 01221-020 - São Paulo - SP - Tel/Fax: (55 11) 5051-2165 - E-mail: ivobf@dialdata.com.br
The present study was presented as a poster at the 35° Congresso Brasileiro de Otorrinolaringologia, held in Natal (RN), on October 18, 2000.
Article submitted on November 20, 2000. Article accepted on January 15, 2001.


