INTRODUCTIONThe number of people with positive HIV grows annually in Brazil3 and all over the world9. According to estimates of the World Health Organization, more than 16 thousand people are infected by HIV every day around the world and 1.5 to 2 million die every year as a result of the infection11. The prevalence of otorhinolaryngological affections in AIDS patients varies from 41 to 71%2,4,9. However, the literature does not address frequency and characteristics of these diseases in early stages of the HIV infection. Rhinosinusitis is the most common manifestation, with prevalence of 20 to 60%4,12. Previous knowledge of otorhinolaryngological manifestations in HIV-infected patients is important for early diagnosis, better therapy and prevention of its dissemination.
The report of the present clinical case aimed at highlighting the presence of fungal rhinosinusitis as the first manifestation of HIV virus/AIDS, stressing the importance of diagnosing these affections in order to provide early diagnosis and better prognosis.
REVIEW OF LITERATURE -DIFFERENTIAL DIAGNOSISThe literature clearly shows that more than 40% of the patients with Acquired Immunodeficiency Syndrome AIDS present head and neck manifestations, among them, rhinosinusitis5,9,14. Patients with AIDS and HIV with rhinosinusitis are susceptible to common infectious organisms that are normally treated conservatively. The commonest etiology, based on routine culture, is bacterial6,7,8,10,15, but patients may also be infected by virus, fungi and parasites5, which despite their rarity, are increasing in frequency.
In 1990, Meiteles and Lucente12,14, in a review of the literature about microorganisms found in HIV infected patients detected, in addition to regular causes, a number of opportunist infections, including infections by Cryptococcus, Alternaria and Pseudallescheda14. Aspergillosis has already been found in patients with HIV6 and associated with Pseudallescberia boydii in patients with AIDS6.
Pseudallescberia boydii (Petriellidium boydii), is a soil saprophyte, ubiquinone, and rarely found as the main agent of fungal rhinosinusitis13; it is introduced in the body by cutaneous inoculation leading to infection of soft tissues of lower limbs ("mature foot') or by the respiratory tree13,15.
Gluckman et al. in 1977 reported the first cases of paranasal sinusitis caused by Pseudallescbeda boydii in a diabetic patient. In 1978, Mader et al. reported a case of sphenoid sinusitis in a immunocompetent 33 year-old woman and Hecht and Montgonaerie described a case of invasive maxillary sinusitis in a 20-year-old man with acute lymphocytic leukemia. Winn et al. (1983), Morgan et al. (1984) Stamm and Frable (1992) reported cases of invasive paranasal sinusitis by Pseudallescberia boydii in immunocompetent hosts13. Watters and Milford (1993) reported a case of sphenoid sinusitis by Pseudallescheria boydii in a 52-year-old woman who was not immunocompromised15.
Pseudallescheria boydii has been rarely isolated in cultures from paranasal sinuses punch of patients with community-acquired acute sinusitis6. Only two cases of infection by Pseudallescheria boydii in patients with AIDS have been reported, both of them fatal6. Pseudallescheria boydii is rarely invasive and most of human infections lead to mycetoma or fungus ball15.
Differential diagnosis of fungal rhinosinusitis caused by Pseudallescheria boydii and Aspergillus is based on the fungus culture, because histopathological exam does not differentiate hyphae of Pseudallescberia boydii from those of Aspergillus. Both have septated and branched hyphae that may present bulb areas15. Histologic exam is important to detect invasion of adjacent tissues15 and it is necessary to differentiate invasive fungal disease from fungal ball or invasive fungal sinusitis10.
Bacterial rhinosinusitis may be present at any stage of they HIV disease, but fungal rhinosinusitis seems to be present when CD4 lymphocyte T count is below 150mm³10. The most common fungal infection of paranasal cavities is Aspergillosis, which responds to Amphotericin B. Different therapeutic options have been used against Pseudallescberia boydii. Miconazole should be the preferred drug because Pseudallescberia boydii is relatively resistant to Amphotericin B15. Cetoconazole is another recommended agent6. Itraconazole has been effectively used6. Treatment of itraconazole for fungal rhinosinusitis caused by Aspergillus is limited and it has been approved by the FDA - Food and Drugs Administration as second line therapy for invasive aspergillosis in patients that do not tolerate Amphotericin B or in those whose treatment has failed10.
Considering the high incidence of otorhinolaryngological manifestations in AIDS patients and the fact that they may be the first manifestation of the disease, we realized that for patients who have persistent paranasal sinuses infections, the diagnosis should be considered, even in the absence of other manifestations of the disease. If there is no improvement after initial treatment, we should indicate CT scan because it is the first step to assess severity and extension of the disease10. Early intervention for collection of material should also be performed, using techniques for aerobic, anaerobic, fungal, virus and mycobacterium agents. Fungal rhinosinusitis should be treated with surgical drainage and aeration of cavities14,15. Extensive and complete surgical debridement is essential, combined with anti-fungal therapy.

Figure 1. CT scan of paranasal sinuses showing affection of maxillary, ethmoid and sphenoid sinuses and nasal fossa on the left.
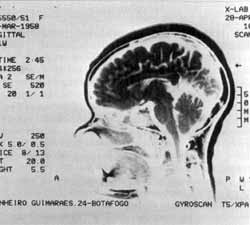
Figure 2. Magnetic nuclear imaging did not show affection of encephalic structures.
FNVB, a black female 36-year-old patient, from Rio de Janeiro, came to the Otorhinolaryngological service in January 1993 presenting complaints of left nasal obstruction, followed by nasal discharge for four months. The exam revealed mucoid retronasal discharge, paleness and hypertrophy of inferior and middle conchae, especially on the left, and septal deviation to the same side. Simple radiological study showed diffuse velamentum of frontal, ethmoid and maxillary sinuses on the left and hypotransparency of sphenoid sinuses. She was medicated with systemic nasal decongestant, nasal lavage with sterile solution, topic corticoid, sulfamethoxazole and trimethoprim and mucolytic for 14 days. Radiological follow-up showed velamentum of cavities and destruction of septum in the ethmoid sinus. The patient was medicated with ciproflaxacin and we ordered a CT scan of paranasal sinuses. The exam revealed heterogeneous areas of high and low density, with contrast, that partially occupied the maxillary sinus and the nasal fossa on the left, ethmoid and lateral wall of sphenoid on the left, plus osteogenic reaction of bone limiting of affected paranasal sinuses, suggesting granulomatous chronic inflammatory reaction (Figure 1). We conducted intranasal maxillary antrostomy under sedation and local anesthesia, and biopsy of the lesion. Histopathological and histologic exams identified mucus lumps involving red cells, pyocytes, colonies of bacteria and structures similar to fungi, in addition to bone fragments with necrosis. The fungi culture showed Pseudallescheria boydii. MRI discarded the affection of encephalic structures (Figure 2). We ordered serologic test for HIV I and II and the result was positive. The patient was submitted to endoscopic surgical procedure for cleaning of cavities and administration of systemic anti-fungal agents - oral Itraconazole 200 mg/day for 30 days.
CT scans conducted annually up to three years after the surgery show total recovery of the nasosinusal mucosa with widely open cavities and no sign of recurrence of the disease (Figure 3).
DISCUSSIONRhinosinusitis is a common clinical problem in patients infected by HIV and it has been considered a potential definer of AIDS. Fungal rhinosinusitis has been reported in HIV-infected patients when the count of lymphocytes T CD4 is below 150mm3,10. Cases of fungal rhinosinusitis by Pseudallescheria boydii described in the literature occurred in patients that complied with the criteria of AIDS according to the definition proposed by CDC (Centers for Disease Control). There are three cases of sinusitis by Aspergillus in AIDS patients associated with Pseudallescberia boydii6.
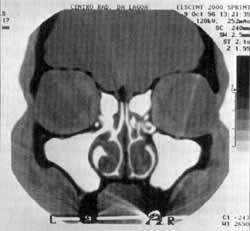
Figure 3. CT scan of paranasal sinuses three years after surgery, revealing ample cavities, with no recurrence of nasosinusal disease.
In our case, the patient had an episode of rhinosinusitis that did not respond to regular therapy for treatment of bacterial etiology, which made us suspect of an atypical etiological agent and we ordered serology of HIV and assessment of immune status. Serology was positive for HIV. The number of lymphocytes was normal, with 850cel/mm³ of CD4 T and 1,632mm³ of CD8 T, showing a reversion - a significant increase of CD8 lymphocytes T The patient had not presented any other HIV AIDS manifestations up to that point.
The diagnostic investigation/biopsy, histopathological and histologic studies and fungal culture allowed us to confirm fungal rhinosinusitis caused by Pseudallescberia boydii, which had only been described associated with Aspergillus in patients with HIV-AIDS, in cases of invasive sinusitis in immunocompromised and immunodepressed patients. The approach with CT scan and MRI showed that the disease was limited to the paranasal cavities and it was not an invasive form of the disease.
Surgical treatment should always be indicated with drainage and aeration of paranasal cavities. Systemic antifungal therapy for Pseudallescheria boydii is indicated because the fungus may invade tissues and spread outwards the paranasal cavities, and cetoconazole and nazole are the adequate agents to be used. In invasive sinusitis by Pseudallescheria boydii, the preferred drug is oral cetoconazole.
In our case, the identification of etiological agent and the surgical therapeutic approach were similar to other cases reported in the literature. Systemic therapy with itraconazole, although it is not the preferred drug, resolved the case probably because the disease was limited to the paranasal sinuses, in addition to the fact that we used the appropriate surgical approach and the immune status of the patient was good. In the annual three year follow-up, there was no evidence of recurrence of the disease.
FINAL COMMENTSRhinosinusitis in patients with HIV is a common fact. The incidence of atypical and opportunist agents has been observed. The report of such cases attracts out attention to the fact that in case of resistance to conventional treatment, surgical interventions to collect material for culture and drainage of cavities are indicated to define the final diagnosis.
We reported a case of non-invasive fungal rhinosinusitis by Pseudallescberia boydii in a HIV infected patient, with no other manifestations of HIV AIDS. As far as we know, this is the first report of such a type of case in the literature.
REFERENCES 1. BOHADANA, S. C.; LIMA, S.; MAIA, L. M. S. V; GONÇALEZ, F.; SILVEIRA, E. G. C.; JÚNIOR, O. M.; RAUSIS, M. B. G.; SILVEIRA, J. A. M. - Surdez Súbita como Primeira Manifestação da Síndrome da Imunodeficiência Adquirida - Rev. Bras. de Otorrinolaringol., 60 (2) : 144-8, 1998.
2. BORGO, del C.; FORNO, del A.; OTTAVIANI, F.; FANTONI, M.- Sinusitis in HIV -infected Patients -J. Chemotherapy, 9 (2): 83-88-1997.
3. GONCALVES, D. et al. - Manifestações Otorrinolaringológicas em Pacientes HIV - Soropositivos - Rev. Bras. de Otorrinolaringol., 60 (4): 407-8, 1994.
4. GONÇALVES, D. U.; TOLEDO JÚNIOR, A. C.; BECKER, C. G.; GONÇALVES, T M. L.; GRECO, D. B. - Manifestações Otorrinolaringológicas em pacientes HIV Soropositivo. Rev. Bras. Otorrinolaringol., 60 (4): 267, 1994.
5. MEITELES, L. Z., MD; LUCENTE, F. E., MD - Sinus and Nasal Manifestations of the Acquired Immunodeficiency Syndrome. Ear, Nose and Throat Journal, vol. 69 - July, 1990.
6. MEYER, R. D.; GAULTIER, C. R.; YAMASHITA, J. T.; BABAPOUR, R.; PITCHEN, H. E.; WOLFE E R. - Fungal Sinusitis in Patients With AIDS: Report of 4 cases and Review of the Literature -Medicine, 73 (2), 1994.
7. MILGRIN, L. M., MD; RUBIN, J. S., MD; SMALL, C. B.; MD. - Mucociliary Clearance Abnormalities in the HIV Infected Patients: A Precursor to Acute Sinusitis Laryngoscope, 105, 1995.
8. MOSS, R. B.; SCOTT, T. A.; GOLDRICH, M.; PITALE, M.; DANIEL, A.; LEBOVICS, R.; WALKER, R.; IGARASHI, Y; KALINER, M. A. - Nasal Mucosal Cells in Human Immunodeficiency Virus Type I - Seropositive Patients with Sinusitis -Journal of Clinical Laboratory Analysis, 10: 418 -422, 1996.
9. MUNHOZ, M. S. L. et al - Manifestações Otorrinolaringológicas em Pacientes com Síndrome da Imunodeficiência Adquirida (SIDA) - Rbm - Otorrinolaringologia, 1 (1): 5457, 1994.
10. MYLONAKIS, E., MD, PH.D, RICH, J., MD, M. P H., SKOLNIK, P R. MD, PH.D; RICH, J., MD, M. E H.; SKOLNIK, P. R., MD; DE ORCHIS, D. F., MD, FLANIGAN, T, MD. - Invasive Aspergillus Sinusitis in Patients with Human Immunodeficiency Virus Infection - Rhinology . 33, (1), 1995.
11. RACHID, M.; SCHECHTER, M. - Manual de HIV /AIDS 3ª edição, Rio de Janeiro - Revinter, (83-87), 1998.
12. ROSSI, R. M., MD; WANKE, C., MD; FEDERMAN, M., PH.D - Microsporidian Sinusitis in Patients With the Acquire Immunodeficiency Syndrome -Laryngoscope, 106: 966-971, 1996.
13. STAMM, M. A., MD; FRABLE, M. A., MD; RICHMOND, VA -Invasive Sinusitis Due to Pseudallescheria boydii in an Immunocompetent Host - Soutbern Medical Journal - 85 (4), 1992
14. UPADHYAY, S., MD; MARKS, S. C., MD; ARDEN, R. L., MD; CRANE, L. R., MD; COHN, A.M., MD - Bacteriology of Sinusitis in Human Immunodeficiency Virus-Positive Patients: Implications for Management -Laryngoscope, 105: 1058 - 1060, 1995.
15. WATTERS, G. W R., F. R. C. S.; MILFORD, C. A., F. R. C. S. - Isolated Sphenoid Sinusitis Due to Pseudallescheria boydii - The Journal of Laryngology and Otology - 1993, 107, 344- 346, 1993.
* Postgraduate of the Discipline of Allergy and Immunology at Universidade do Rio de Janeiro - UNI-RIO. Postgraduate in Otorhirnlaryngology at Universidade do Rio de Janeiro - UNI-RIO. Physician with Clinica Sensorium.
** Full Professor of Allergy and Immunology at Universidade do Rio de Janeiro - UNI - RIO.
*** Joint Professor of the Discipline of Otorhinolaryngology at Universidade do Rio de Janeiro - UNI-RIO.
Study conducted at Clínica Sensorium - Rio de Janeiro
Address for correspondence: Dra Rosane Clara C. Victorino - Av. Rio Branco, 156 - Grupo 2312 - Centro - 20040-030 Rio de Janeiro /RJ. Tel: (55 21) 533-1070 - Fax: (55 21) 262-9793. Article submitted on July 28, 2000.
Article accepted on December 7, 2000.


