INTRODUCTIONSnoring is sound produced during sleep through the vibration of the pharynx soft parts (uvula, palate, tonsil pillars, tongue base) during the passage of air and occurs owing to the increased resistance to permeability of the airflow through the upper airways 1. It affects adults and children and can lead to social problems: when associated with frequent waking during the night and daily drowsiness, with normal polysomnographic findings it is characterized as upper airway resistance syndrome 2, and when related to Obstructive sleep apnea-hypoapnea syndrome (OSAHS) it can lead to co-morbidities. It is a very subjective complaint, since it can be influenced by the reporters' emotions. The information is provided by the patient or the accompanying person, which makes the complaint under or overestimated depending on the sleep quality of the other 3. Literature studies report that when comparing snoring complaints reported by the patient, spouse or a third-party not related to the patient, there is discrepancy of information 4.
The literature also informs that the incidence ranges from 28% in female population to 44% in males 5-8 and these values tend to increase with aging up to the 7th decade of life, in which it can reach 84% in men and 73% in women of this age range 8. Even though occurrences of snoring and apnea have been recognized for quite a long time (there are reports of 360 BC), in the past 30 years they have gained body in the scientific world 1. Many clinical and surgical treatment approaches were proposed as of the beginning of the 50's and they were largely disseminated in the 80's 9. The basis for treatment, regardless of the surgical technique used, are the same: expend the air column to the lungs, reducing airflow resistance, be it by removal of soft tissues (palate, pillars, tongue), be it by displacement of bone structure (mandible, maxilla). Among the described techniques we can include osteotomy with maxillomandibular advancement and its variations 10, hyoid suspension 11, tracheostomy 12, 13, adenoidectomy and/or tonsillectomy, nasal surgery, somnoplasty, CO2 laser, uvulapalatopharyngoplasty (UPPP)9 and palate partial resection (PPR)14, which is the purpose of our study. The objective of the study was to assess the results of snoring remission, as well as postoperative pain and complications with the use of PPR described by Quesada et al. and Perelló14 in patients complaining of snoring.
MATERIAL AND METHODSWe conducted a retrospective study of 28 patients submitted to partial palate resection (PPR) between April 1994 and August 2000, being that 5 patients did not meet the inclusion criteria. Ages ranged from 20 to 75 years, mean age of 46.7, being that most of them (17) were aged between 30 and 50 years. There was predominance of male patients, including 25 male patients and 3 female patients.
All patients were assessed comprising the following parameters: paranasal sinuses and nasal fossa CT scan, polysomnography and complete ENT examination. In polysomnography, the parameters used were: apnea/hypoapnea index/hour (IAH), oxygen minimum saturation (satO2), and snoring intensity. Apnea and hypoapnea were defined as total or partial cessation, respectively, of nasal/oral airflow for over 10 seconds and according to the American Academy of Sleep Medicine (AASM), OSAHS is characterized by recurrent episodes of partial or total obstruction of upper airways during sleep 15.
IAH was classified as normal when there are five events per hour, mild for 5 to 15 events, moderate for 15 to 30 events, and severe when it exceeds the number of 30 events per hour 15. Snoring intensity was classified as follows 1:
Grade I: occasional snoring, in supine position, associated with excessive tiredness, alcohol and/or food intake.
Grade II: louder and frequent snoring, any position, which can be heard from the other rooms in the house.
Grade III: excessively loud snoring, which can be heard from anywhere in the house, normally associated with OSAHS.
As to oxygen saturation, it was classified as normal when above 90%, mild unsaturation 85% to 89%, moderate 65% to 84%, and mild below 85%.
The physical examination of patients submitted to this technique found soft palate and/or posterior pillar hypertrophy redundant in all patients, nasal septum deviation in 18 cases (64%), lower turbinate hypertrophy in 3 (11%), and palatine/lingual tonsil hypertrophy in 1 case (3.5%). Nasosinusal findings were confirmed by paranasal sinuses CT scan.
Polysomnography revealed mild/normal IAH in 22 patients (78.5%), moderate in 4 (14%) and severe in 2 (7%). Sat O2 was normal in 19 cases (68%), mild hypoxia in 6 (21%) and severe in 3 (11%). Snoring grade III was observed in 7 cases (25%), grade II in 5 cases (18%) and grade I in 16 cases (57%).
We included in the study only patients with mild or normal IAH, BMI<25 with no clinical signals of significant deprivation of sleep according to Epworth scale and without any other comorbidity. We excluded from the 6-month follow-up 5 patients that presented comorbidity, being 2 with severe IAH and 3 with moderate IAH. Only 1 patient with moderate IAH was included since he did not present clinical symptoms of excessive daily drowsiness.
Technique1. Definition of the hard palate limit (with electrical knife) as a reference point. tonsillectomy, if present;
2. Partial resection of uvula (Figure 1);
3. Eversion of uvula stump to define the limits of mucous displacement so as to have 1.5 to 2.0 cm long left in the soft palate and 1cm lateral from the last upper molar;
4. Displacement with electrical knife of the mucosa and submucosa of the oral aspect of the palate (Figure 2);
5. Eversion and suture with vicryl 3.0 with separated stitches (Figure 3), showing final aspect without wounded area or palate muscle resection (Figure 4).
We assessed postoperative pain using patients' reports, defining use of analgesics and reintroduction of regular diet, early complications (hemorrhage, hematoma, airway obstructive edema) and late complications (velopharyngeal insufficiency, changes in voice, stenosis, myoclonus, loss of taste, bacterial infections, nasal reflux of foods)16 and snoring remission. These data were subjectively assessed through information provided by the patients and their family members. We did not perform polysomnography during the six-month follow-up because the objective of the study was to assess only resolution of snoring.
RESULTSPain remission with total discontinuation of analgesics occurred within one week for 6 patients (21%), 2 weeks for 19 patients (68%) and 3 weeks for the other three patients (11%). As to introduction of general diet, they were all instructed to keep a liquid and/or paste diet for the first week to reduce the risk of complications and, after this period, they were allowed to start their regular diet. By the end of the 2nd week, they had all restored their regular habitual diet.
Snoring improvement, after six months, was total in 12 cases (42%), partial in 9 (32%) and unchanged in 2 (7%), and five patients did not complete the study.
Only one patient presented transient rhinolalia as postoperative complication and none presented other complications up to 6 months postoperatively. None of them were reoperated.
DISCUSSIONSurgical therapy for snoring consists of treatment of palate hypertrophy, tonsil and nasal surgery. Among the described palate techniques, surgery with CO2 laser, somnoplasty, uvulopalatopharyngoplasty and partial palate resection are the most frequently referred. The approach of the palate to treat snoring was initially described in the 50's and introduced in the USA in the 80's 9. Isolated snoring does not normally cause systemic repercussions, but apnea can imply significant impairment in quality of life (tiredness, daily drowsiness, irritability, changes of mood, and cognition impairment)1, general complications (hypertension, arrhythmia, AMI, CHF, night sudden death)1 and increased risk of car accidents 17, deserving special attention. In children, other manifestations are impaired weight and height gain, growth of the face mid-third and compromise of school performance.
In the present study, we considered only the snoring complaint of patients in order to direct to the resolution. We studied one well-known surgical technique and followed it up for 6 months, a period in which our study reproduced the results found in the world literature. In some longer studies they showed that success rates of UPPP decreased with time and then stabilized. Levin and Becker18 assessed 69 patients in a 5-year follow-up and observed that after 13 months, the rate of total or partial remission of snoring reduced from 87% to 46%. Studies with other types of palate surgery did not show better results than the ones reported here, and there was no technique that produced 100% success. The advocators of each technique present potential advantages of the procedures, and there is no final consensus about the topic in the literature.
CONCLUSIONThe present study followed up for 6 months 23 patients submitted to partial palate resection for snoring management, through the technique proposed by Quesada and Perelló. It presented satisfactory results in snoring remission, low risk of intra and postoperative complications and total improvement of pain within two weeks for most of the patients, confirming it is a good alternative to manage this type of affection.

Figure 1. Partial uvula resection at the level it is sutured on the anterior surface of the palate.
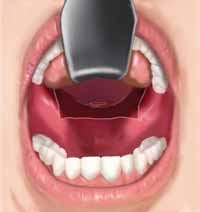
Figure 2. Anterior mucosa of the soft palate, with no muscle tissue loss.
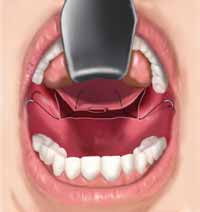
Figure 3. Eversion and suture.

Figure 4. Final aspect.
1. Pontes PAL. Ronco e Síndrome da Apnéia Obstrutiva do Sono (SAOS). In: Stamm A. ed. Rinologia 2000; São Paulo: Revinter; 2000:315-319.
2. Guilleminaut C, Stools R, Clerk A et al. From obstructive sleep apnea syndrome to upper airway resistance syndrome: consistency of daytime sleepiness. Sleep 1992; 15:S13-S16.
3. Wiggins CL, Schmidt-Nowara WW, Coultas DB, Samet J. Comparison of self- and spouse reports of snoring and other symptoms associated with sleep apnea syndrome. Sleep 1991; 13:245-52.
4. Hoffstein V, Mateikas S, Anderson D. Snoring: is it in the ear of the beholder? Sleep 1994;17:522-6.
5. Lugaresi E, Cirignotta F, Montagna P, Sforza E. Snoring: pathogenic, clinical, and therapeutic aspects. In: Kryger MH, Roth T, Dement WC, eds. Principles and practice of sleep medicine. Philadelphia: WB Saunders; 1994: 621-9.
6. Lugaresi E, Cirignotta F, Coccagna G, Piana C. Some epidemiological data on snoring and cardiocirculatory disturbances. Sleep 1980; 3:221-4.
7. Young T, Palta M, Demsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993; 328:1230-5.
8. Norton PG, Dun EV. Snoring as a risk factor for disease: an epidemiological survey. BMJ 1984; 291:630-2.
9. Ikematsu T, Fujita S, Simmons FB, et al. Uvulopalatopharyngoplasty: variations in snoring and sleep obstructive apnea. In: Fairbanks DNF, Fujita S, eds. Snoring and sleep obstructive apnea, 2nd ed. New York: Raven Press; 1994:97-146.
10. Riley RW, Powell NB, Guilleminaut C. Obstructive sleep apnea syndrome: a review of 306 consecutively treated surgical patients. Otolaryngol Head Neck Surg 1993; 108:117-25.
11. Riley RW, Powell NB, Guilleminaut C. Obstructive sleep apnea and the hyoid: a revised surgical procedure. Otolaryngol Head Neck Surg 1994; 111:717-21.
12. Miller FR, Eliacgar I, Tucker HM. Technique, management, and complications of the long-term flap tracheostomy. Laryngoscope 1995; 105:543-7.
13. Sahni R, Blakeley B, Maisel RH. Flap tracheostomy in sleep apnea patients. Laryngoscope 1985; 95:221-3.
14. Quesada P, Pedro Botet J, Fuentes E, Perelló E. Resección parcial del paladar blando como tratamiento del sindrome de hipersomnia y respiración peródica de los obesos. ORL Dips 1977; 5:81-8.
15. AASM Task Force. Sleep 1999; 22(5): 667-89.
16. Pinto JA, Colombini NEP, Faller GJ. Complicações em cirurgias para apnéia obstrutiva do sono. In: Stamm A. ed. Rhinology 2002; São Paulo: Komedi; 2002:121-31.
17. Phillipson EA. Sleep apnea: a major public health problem. N Engl J Med 1993; 382:1271-3.
18. Levin BC, Becker GD. Uvulopalatopharyngoplasty for snoring: long-term results. Laryngoscope 1994; 104:1150-2.
1 Resident physician in Otorhinolaryngology.
2 Preceptor of the Residence Program.
3 Coordinator of the Residence Program.
Service of Otorhinolaryngology, Hospital Beneficência Portuguesa - Clínica Ivan F. Barbosa.
Address correspondence to: Luis Francisco de Oliveira - R. Maestro Cardim, 770 Bela Vista Sao Paulo SP 01320-001.
Tel (55 11) 288-0899 - Fax (55 11)3253-0705 - E-mail:lf_otorrino@uol.com.br
Study presented as free communication at 36º Congresso Brasileiro de Otorrinolaringologia - Florianópolis/SC, on 22/11/2002, room 12.


