INTRODUCTIONRhinosinusitis can be described in general as an inflammation of the nasosinusal mucosa in response to the action of infectious or traumatic events, exposure to chemicals or even the action of allergens triggered by an inflammatory status of the mucosa. Such event initially has acute characteristics that can resolve spontaneously or by using drugs that will interact to normalize the nose and paranasal sinuses mucosa. However, in some cases, it does not occur and persistence of such affections leads to chronic character of the disease.
Nasosinusal mucosa is specialized, known as being recovered by respiratory epithelium, which is found in the tracheobronchial tract, as well as in the middle ear. It has specialized structures in its composition, such as columnar hair cells, seromucous glands, which together with goblet cells, produce mucus; the whole set will form the mucociliary system of the epithelium, an important mechanism for airway defense. Any failure in this system will increase morbidity of the structures of the region, leading to installation of inflammatory processes associated or not with infection 1.
Therefore, the knowledge of the affections suffered by the epithelium during the process of chronification explains the reason why in some cases there is easy installation of inflammatory conditions resistant to clinical or surgical treatment. Such affections can be related to inability of the mucosa to maintain the defense mechanisms. Our purpose was to study the main histological and ultrastructural affections of the maxillary sinus mucosa of patients with chronic rhinosinusitis and nasosinusal polyposis submitted to functional endoscopic sinus surgery.
MATERIAL AND METHODThe studied group comprised 10 patients seen in the Ambulatory of Rhinosinusitis, Department of Ophthalmology and Otorhinolaryngology, Medical School of Ribeirao Preto, University of Sao Paulo (FMRP, USP), approved by the Research Ethics Committee, H.C.R.P., according to protocol nº 1930/97.
Patients were submitted to endoscopic surgery with diagnosis of chronic rhinosinusitis (CR) or nasosinusal polyposis (NP) refractory to previously attempted clinical treatment, using clinical history, nasofibroscopy and computed tomography (CT) of the paranasal sinuses, presenting as mucous thickness of maxillary sinus, total or partial opacification of ostiomeatal complex and opacification with soft part density.
In the studied group, 40% were female and 60% were male subjects, aged 11 to 73 years.
We excluded patients submitted to previous nasal and/or paranasal surgery and those with associated diseases, such as cystic fibrosis, primary ciliary diskinesia, immunodeficiency, intolerance to acid acetyl-salicylic and severe asthma.
The control group comprised 4 cadavers submitted to necropsy by the Service of Death Investigation, Department of Pathology, FMRP, USP, with no history of rhinosinusitis and death not caused by infection. They were submitted to nasofibroscopy, did not present anatomical abnormalities or suspicion of respiratory diseases.
The following preoperative tests were ordered: complete blood count, coagulation time and total IgE dosage, in order to differentiate patients who were allergic. Skin tests were conducted by the Department of Immunology, FMRP, USP during the clinical hospitalization of the patients.
The mucosa was removed during the surgery from the superior-lateral wall of the maxillary sinus. We used a curved Blakesley-Wilde clamp, and the sample was treated according to a standardized method to prevent mistakes resulting from the procedure. The following steps were followed:
Fixation of the fragment in a solution of glutaric aldehyde at 3.0% in buffer solution of Sorensen for 3 to 4 hours. The samples were directed to transmission electron microscopy and divided into smaller fragments and after being washed in buffer solution, they were soaked in a solution of osmium tetroxide at 1% in Sorensen buffer 0.1 Molar for 2 hours at 4o C temperature. Dehydrated, fragments were infiltrated and included in Resin Araldite 6005, sectioned with an ultra-microtome (Reichert UltraCut S) at initial thickness 0.5 micrometers and prepared in histology slides. The sections were stained with toluidine blue solution at 1.0% in borax and stored for the light microscopy analysis. After analysis and selection of sections from the fragments, the blocks were readjusted and submitted to ultrafine section (60-70 nanometers) which were collected in a copper grip and submitted to a process of contrast using uranil acetate and lead citrate, observed and electro-photographed with a Microscope Philips 208 operating at 80 Kv in Kodak 4489 plates at variable magnification.
Fragments directed to scanning electron microscopic (SEM) remained in the glutaric aldehyde solution at 3.0% for 3 hours, washed in buffer Sorensen phosphate to remove free aldehyde. Next, they were immersed in osmium tetroxide solution at 1.0% in buffer phosphate 0.1 molar at 4o C temperature, dehydrated in ethanol and dried by the critical point in CPD-030 Bal-TEC. The samples were prepared in appropriate supports using a conductive paste (Conducting Graphite Paint / Laad Research Industries), recovered by gold in a unit SCD-050 BAL-TEC, examined and electro-photographed in a scanning microscope JEOL JSM 5200 at variable magnifications using film Verichrome Pan Kodak VP 120.
The semi-fine sections stained with toluidine blue served as the basis for the light microscopic study. Based on them, we classified the type of epithelium or the mucous lining based on number of cell layers (simple, stratified, or pseudo-stratified) and the type of more superficial cell (squamous, columnar). They were photomicrographed in a photomicroscope Zeiss with Apo 40 or PlaApo 63 objectives and Kohler light and ProImage 100 film.
RESULTSWe studied 10 patients with NP and CR. Five of the patients had allergic complaints or previous history of allergy in childhood. None of the patients had family history involving allergy or similar sinus disease. Patients were submitted to serum total IgE dosage, but only six of them presented data different from the normal pattern according to the Laboratory of Immunology, HCFMRP-USP. Seven patients presented positive skin test for some tested allergens (Table I). In the classification of patients in groups of allergic and non-allergic, we used three parameters: allergic history, skin test and total IgE dosage. Patients with positive clinical history to allergy or positive skin test were considered as part of the allergic group.
At the surgical act, we collected secretion and mucosa and sent them to culture for aerobe, anaerobe and mycology conducted at the Laboratory of Microbiology, HCRP. Out of 10 studied patients, eight had positive results being that there was always an association of two or more microorganisms present. The microorganisms found in 8 patients with positive culture are demonstrated in Table II.
HISTOLOGICAL AND ULTRASTRUCTURAL STUDYThe control group, comprising four cadavers, had many samples exhaustedly studied under light, electron and scanning electron microscopy. All of them presented columnar ciliary pseudo-stratified epithelium (normal respiratory epithelium), thin mucosa with few goblet cells, and a single layer of epithelium over a delicate basal membrane. Lamina propria, also thin, comprised loose connective tissue with disseminated leukocytes. SEM showed intense ciliary surface, cilia with normal morphological aspect (Figure 1).
The studied group comprising 10 subjects, had samples removed during the functional endoscopic surgery performed. Many samples of each patient were similarly studied. The distribution of the epithelium can be found in Table III. Two patients presented normal respiratory epithelium on the surface, but curiously the lamina propria was not normal. There were areas of inflammatory process (with absence of organization of the cell interstitium, presence of disseminated cell debris, cell population comprising plasmocytes and macrophages and area of chronic inflammatory process, with fibrosis of the lamina propria close to the epithelium, presence of elements of destruction and cleaning, intense aggression to the mucosa, diversity and abundance of cell figures. Two patients presented a mucosa with atypical respiratory epithelium: an important reduction in number of ciliary cells, with increase in goblet cells throughout the epithelium and extruding on the surface, and increased intercellular spaces. Basal cells presented a different morphological aspect: they were flatter (Figure 2). The lamina propria presented with areas of marked inflammation, rich cell diversity and sometimes areas of fibrosis. Three patients presented mucosa with metaplastic epithelium. In two cases, there was one single layer of flat cells, but the cuboid cells presented secretion granules; one case with squamous stratified epithelium with very increased intercellular spaces (Figures 3 and 4). Lamina propria presented rich cell diversity, with areas of acute and chronic inflammatory process. The three last patients presented different types of epithelium covering the mucosa of the maxillary sinus: areas of metaplastic epithelium intertwined with areas of respiratory epithelium completely deprived of cilia. We observed a significant reduction of number of ciliary cells, number of cilia, and cells with many granules of secretion on the apical surface (Figure 5). The lamina propria presented areas of acute and chronic inflammatory process.
DISCUSSIONNasosinusal mucosa inflammation in acute or chronic conditions has been discussed in the ENT literature under different aspects: characteristic clinical pictures, distribution by age, gender and ethnic group, allergic history and associated underlying diseases, which would facilitate the development or maintenance of mucosa affection, trying to specify the possible groups in which there is higher incidence of affection.
Patients assessed in this study had a distribution of age range compatible with the one found by Toskala et al. (1995)2, mean age of 37 years, and Guo et al. (1997)3, mean age of 45 years. In our study, 40% of the cases were aged between 31 and 45 years.
It is interesting to note that in the three first decades of life the cases represented only 30% of subjects in our study. CR is more predominant after the 3rd decade of life, a fact compatible with the reports previously referred. Our group comprised 6 male patients, amounting to 60% of the total. This result is similar to that referred by Guo et al. (1997)3, but does not follow the results of the studies conducted by Toskala el al. (1997)4, Al Rawi et al. (1998)5, in which female gender amounted to 75% and 56.5% of the cases, respectively. Therefore, it is difficult to infer about the incidence concerning gender predominance since our study was conducted in a small sample and there is still controversy in the literature.
The main complaints reported by the patients were nasal obstruction and nasal secretion, amounting to 70% of the isolated or combined complaints. In a smaller proportion, about 30% of the complains were of headache, sneezing and nasal pruritus. These data are confirmed by the study conducted by Gaffar et al. (1998)6, which describes chronic nasal congestion, rhinorrhea, headache, chronic cough ad anosmia as the complaints present in these conditions. Nasal obstruction as one of the main complaints can be easily explained, since at nasofibroscopy, as well as in radiological studies, we can detect the presence of increased nasal concha associated or not with degeneration of nasal mucosa, obliteration of ostiomeatal complex, with presence of polyps or mucosa thickness. Nasal secretion can be sometimes explained by the stasis that occurs associated with obstruction and infection.
ALLERGIC HISTORYThis point has been widely discussed in the literature. The controversy lies in the issue whether allergy is a cause or the main component of the development of chronic rhinosinusitis or its maintenance. In the group of allergic patients, we noticed that the histopathology study presented different types of epithelium in two patients, cuboid epithelium in one patient and respiratory epithelium in two patients. In six cases, the epithelium proved to be secretory to highly secretory and in only one case, it was non-secretory with metaplasia. In the group of patients that presented enhanced allergic response, with no allergic history, we found atypical epithelium that was highly secretory and mixed secretory. The data made us wonder whether allergy or allergic response was one of the factors in maintaining chronic inflammatory pictures based on the histopathological alterations found. The findings were also evident for some authors, who described marked inflammatory infiltrate and abnormalities of cell characteristics in the studied epithelium, such as more secretory cells, reduction of ciliary cells and epithelium structural changes through squamous cell metaplasia 7, 6, 9, 10.
The group of patients considered non-allergic presented normal respiratory epithelium in two cases and secretory squamous epithelium in one case, which presented highly elevated IgE, but skin test was negative and there was non-characteristic allergic history.
MICROBIOLOGICAL STUDYAnother important parameter to analyze with histological abnormalities is the presence of infection in the studied sinus. To that end, we collected secretion during the surgical act. Out of 10 studied cases, only two did not present positive culture. The fact that in our sample there were 80% of cases with presence of infectious process confirms the hypothesis that superimposed infection helps in the perpetuation of the inflammatory process. Together with infection we found epithelia that varied from normal to metaplasia. In addition to highly secretory epithelium, the structure varied from columnar to squamous. Such facts are in agreement with studies already conducted, such as by Toskala et al2(1995) that studied patients with acute and chronic infection and noticed that there was significant increase of non-ciliary cells.
HISTOPATHOLOGICAL STUDYSince there is a massive debate about the importance of allergy in the pathogenesis of CR, we initially decided to divide the allergic patients from non-allergic patients in the groups and studied the possible correspondence between the histological types. Since there were no findings we decided not to further discuss it.
Many authors have reported both in experimental studies with rabbits and in humans that chronic infection causes thickness of the whole mucosa layer. In clinical practice we frequently find polypoid affections of different grades and mucosa thickness of the maxillary and ethmoidal sinuses during paranasal sinuses endoscopic surgeries.
Reimer et al. (1978)11, studied samples of maxillary sinus mucosa with SEM and found areas of non-ciliary epithelium in 12 patients with CR.
Ohashi & Nakai (1983)12 conducted the same study with maxillary sinus mucosa of patients with CR and observed significant increase of non-ciliary cells in the infected mucosa, as well as extrusion of epithelial cells, edema of ciliary membrane, squamous metaplasia and abnormalities in the formation and composition of cilia. Invasion of inflammatory cells in the lamina propria was also described.
Stierna & Carlsöö (1990)10 studied the maxillary mucosa of patients with CR and found areas of hyperplasia with goblet cells in the respiratory epithelium of many of them, as well as squamous metaplasia in the others, but they did not specify nor quantified the cases. They described other findings, such as subepithelial thickness, increase in number of inflammatory cells in the lamina propria and presence of fibrosis.
Min et al., in 19938, also found in their studies a significant reduction of ciliary surface of infected mucosa of rabbits, as well as of morphological distortion of cilia.
All these morphological alterations found by the authors are described but not quantified. Based on inflammatory responses, most authors describe four types of histology pictures in CR: edematous or hyperplastic, infiltrative or granulous, fibrous or mixed 13, 14. However, many histology types are frequently found in one or more samples of the same mucosa.
In our group of patients we found four epithelial histology types. Despite the fact that two of the patients presented mucosa with normal cover layer (typical respiratory epithelium), the lamina propria showed areas infiltrated by inflammatory process, sometimes with marked fibrosis; two patients with atypical respiratory epithelium, in which we could clearly detect the replacement of ciliary cells for increased number of goblet cells that were highly secretory; and three patients with metaplastic epithelium. Despite the fact that the cells were squamous flat cells, they comprised many secretion granules or presented increase intercellular spaces, the last three cases had mixed epithelium: squamous metaplasia and areas of respiratory epithelium, with reduction in the number of ciliary cells and number of cilia in each cell. The most frequent histological type found in the lamina propria was infiltrative and mixed: areas of acute inflammatory process were mixed with areas of chronic process, in which fibrosis was predominant, with large quantity of collage in the interstitium. The cell diversity was rich (neutrophils, monocytes, lymphocytes, plasmocytes, mast cells, eosinophils), demonstrating the presence of many inflammatory cells invading the epithelium. Our results are the same as those reported by the authors above referred, despite the fact that most had studied rabbits' mucosa.
Many studies reported significant increase in number of goblet cells in chronic inflammation of maxillary sinus 13, 15. However, quantitative histology exam of the maxillary sinus mucosa conducted by Tos & Morgensen, in 198416 , pointed towards significant reduction of density of goblet cells in CR. According to the authors, polypoid mucosa and epithelial necrosis, which occur in the earlier stage of the disease (as part of the regeneration process, they become recovered by a new layer of relatively young epithelium, with smaller density of goblet cells), could explain this difference. We found in our sample two cases of goblet cell hyperplasia. All the others presented small amounts of them.
We detected thickness of subepithelial layers many times associated with increased number of inflammatory cells. This thickness has been interpreted as hyalinization of the basal membrane (Nostrand & Goodman, 1976)17 impairing the transportation of fluids, nutrients and protection factors through the epithelium, reducing the mucosa capacity to resist microbiological stress and promote post-inflammatory self-repair 10. The metaplasia and extrusion of epithelial cells observed by us has also been reported by other authors 2, 12, probably caused by infection, virus or bacterial attack.
Even though the patients in this group had been submitted to SEM and TEM we did not detect ultrastructural changes in the morphological aspect of the cilia, as reported by other authors 8, 12.
As demonstrated in our study and by the literature references described here, chronic inflammation of the maxillary sinus can result in significant loss of ciliary mucosa, with development of atypical respiratory epithelium that is metaplastic or mixed. Such affections should be associated with abnormalities in the paranasal sinuses functions.
According to Kaliner et al. (1997)18 affections to the epithelial function can have a significant role in the pathogenesis of CR, not only because of the morphological impairment described, but mainly because of abnormal production of epithelial catabolites, which could have an essential role in cell inflammation. Epithelial cells are capable of producing cytokines and stimulating factors of the granulocyte colonies - macrophages. An impaired production of these cytokines would affect recruiting, survival and activation status of inflamed leukocytes. Moreover, impaired production of nitric oxide by the epithelium could be important in antibacterial protection. It was recently demonstrated that nitric oxide is produced in large quantities by human sinus healthy epithelium. Owing to its anti-viral and bacteriostactic properties, it has been suggested that nitric oxide has a role in the defense of sinus host.
Based on these observations, Kaliner et al. (1997)18 suggested that the inflammation is influenced by epithelial function abnormalities, and that both are affected by bacterial products that could perpetuate the inflammatory cycle.
Despite the accumulated data so far concerning triggering and perpetuating factors of CR (critical cell elements, cytokines and mediators involved, bacteria, virus, fungal microorganisms or microbial products), research studies are needed to better understand their importance and how such factors act in triggering an inflammatory process.
CONCLUSIONChronic inflammation of the maxillary sinus can result in significant modification of the epithelial cover of the maxillary sinus wall with development of atypical epithelium, which can lead to cases of metaplasia.
Table I- Patients with CR + NP submitted to surgery. Presentation of cases according to history and complementary tests.
* Normal Value: 100 UI/ml
Table II - Microorganisms found in eight patients that presented positive culture.
n= number of positive cultures
Table III - Types of epithelia found in the studied patients.
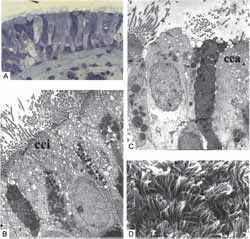
Fig. 1 - Normal respiratory epithelium found in the control group (cadavers). A- LM (light microscopy) (63X); B- TEM: ciliary cells intertwined (cci) with goblet cells (cca) (4,000X); C- TEM: ciliary cell, non-ciliary cell and goblet cell on the surface (4,000X); D- Normal ciliary surface at SEM (3,500X).
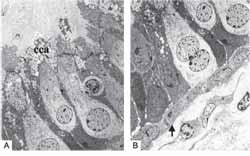
Fig. 2- Patients A- TEM: atypical respiratory epithelium: increase in goblet cells (cca) (2,000X); B- TEM: flat basal cells - arrow (2,000X).
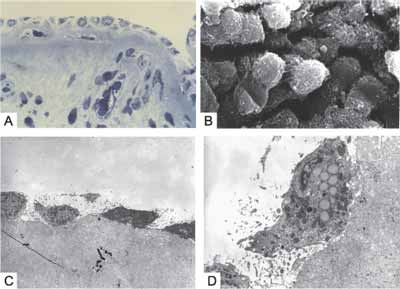
Fig. 3 - Patients - metaplastic Epithelium. A- LO (63X); B- SEM: cuboid cells of the pluristratified metaplastic epithelium, total absence of cilia (3,500X); C- TEM: single layer of flat cells, lamina propria rich in fibrosis (2,500X); D- TEM: metaplastic flat cell rich in secretion granules (8,000X).
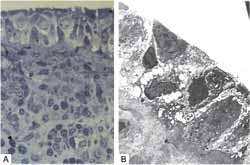
Fig. 4 - Patients - Pluristratified metaplastic Epithelium. A- LM: lamina propria widely inflamed (63X); B- TEM: large intercellular spaces (4,000X).
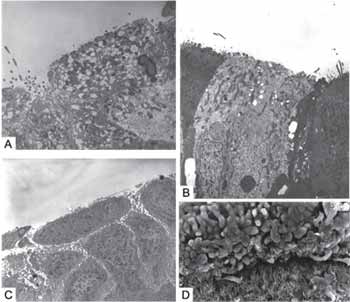
Fig. 5 - Patients - Mixed Epithelium. A- TEM: surface epithelial cell with many secretion granules (5,000X); B- TEM: epithelial surface deprived of cilia (2,500X); C- TEM: squamous metaplasia (4,000X); D- SEM: area with squamous metaplasia, cuboid cells, few ciliary cells, intertwined in an area of many ciliary cells (750X).
1. Demarco, R.C. & Anselmo-Lima, W. T. Fisiologia Nasal. In: Campos, C.A.H.C. & Costa, H.O.O. Tratado de Otorrinolaringologia, 1ª Edição, V. 3, São Paulo, Editora Roca, 2002, 627-639.
2. Toskala, E.; Nuutinen, J.; Rautiainen, M. Scanning Electron Microscopy Findings Of Human Respiratory Cilia In Chronic Sinusitis And In Recurrent Respiratory Infections. The Journal of Laryngology and Otology, 1995, 109: 509-514.
3. Guo, Y.; Majima, Y.; Hattori, M.; Seki, S.; Sakakura, Y. Effects Of Functional Endoscopic Sinus Surgery On Maxillary Sinus Mucosa. Arch Otolaryngol Head Neck Surg., 1997, 123: 1097-1100.
4. Toskala, E.; Westrin, K.M.; Stierna, P.; Rautiainen, M. Ciliary Ultrastructure In Experimental Sinusitis. Acta Otolaryngol. Suppl (Stock), 1997, 529: 137-139.
5. Al-Rawi, M.M.; Edelstein, D.R.; Erlandson, R.A. Changes In Nasal Epithelium In Patients With Severe Chronic Sinusitis: A Clinicopathologic And Electron Microscopic Study. Laryngoscope, 1998, 108: 1816-1823.
6. Ghaffar, O.; Lavigne, F.; Kamil, A.; Renzi, P. Interlenkin-6 expression in chronic sinusitis: colonization of gene transcripts to eosinophils, macrophages, lymphocytes and mast cells. Otolaryngol Head Neck Surg, 1998, 118: 504-511.
7. Westrin, K.M.; Stierna, P.; Carlsöö; Hellström, S. Mucosal Fine Structure in Experimental Sinusitis. Ann Otol Rhinol Laryngol, 1993, 102(8): 639-645.
8. Min, y.g.; lee, y.m.; jung, h. w. et al.: The effect of Ostial Opening on Experimental Maxillary Sinusitis in Rabbits. Rhinology, 1993, 31: 101-105.
9. Fukami, M.; Norlander, T.; Stierna, P. et al. Mucosa pathology of the nose and sinuses: a study in experimental maxillary sinusitis in rabbits induced by Streptococcus pneumoniae, Bacteroides fragilis and Staphylococcus aureus. Am J Rhinol, 1993; 7: 125-132.
10. Stierna, P. & Carlsöö, B. Histopathological observations in chronic maxillary sinusitis. Acta Otolaryngol (Stockh), 1990; 110: 450-458.
11. Reimer, A.; von Mecklenburg, C.; Toremalm, N. G. The mucociliary activity of the upper respiratory tract. III. A functional and morphological study on human and animal material with special reference to maxillary sinus disease. Acta Otolaryngol. (Stockholm), 1978; 355(suppl.): 1-20.
12. Ohashi, Y. & Nakai, Y. Functional and Morphological Pathology Of Chronic Sinusitis Mucous Membrane. Acta Otorhinolaryngol., 1983; 397: 11-48.
13. Schall, LRA. The histology and chronic inflammation of the nasal mucous membrane. Ann Otol Rhinol Laryngol, 1933; 42: 15-38.
14. Mann, W. & Trong, H. D. Vergleichende endoskipische und histologische Befunde bei chronischer Sinusitis. HNO, 1979; 27: 345-7.
15. Albergger, K. W. Abnormal hair like filaments in chronic maxillary sinusitis. Acta Otolaryngol., 1978; 220: 239-249.
16. Tos, M. & Morgensen, C. Muçus Production In Chronic Maxillary Sinusitis. A Quantitative Histopathological study. Acta Otolaryngol. (Stockh), 1984; 97: 115-119.
17. Nostrand Van A.W.P. & Goodman, W. S. Pathologic aspects of mucosal lesions of the maxillary sinus. In: Noyek A.M.; Zizmor, J. eds. Vol 9(1): The otolaryngologic clinics of North America Symposium on the maxillary sinus. Philadelphia. London. Toronto: W. B. Saunders, 1976; 21-34.
18. Kaliner, M. A.; Osguthorpe, J., D.; Fireman, P.; Kennedy, D. Sinusitis: bench to bedside. Current findings, future directions. Otolaryngol Head Neck Surg, 1997, 6(suppl 116): 1-19.
19. Lundberg, J. O.; Farkas-Szallasi, T.; Weitzberg, E. High nitric oxide in human paranasal sinuses. Nat Med, 1995, 1: 370-3.
*Master studies under course, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, FMRP-USP.
**Technician in the Laboratory of Electron Microscopy, Cellular and Molecular Biology and Pathogenic Bioagents.
***Ph.D., Professor, Department of Surgery and Anatomy, FMRP-USP.
****Associated Professor, Department of Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, FMRP-USP.
Study presented at II Congresso Triológico de Otorrinolaringologia da SBORL, Goiania-2001.
Address correspondence to:
Prof Dra. Wilma T. Anselmo-Lima - Departamento de Oftalmologia, Otorrinolaringologia e Cirurgia de Cabeça e Pescoço do HCFMRP-USP, Avenida Bandeirantes n.º 3900 - CEP: 14049-900 Ribeirão Preto - SP -Telefone (0xx16) 602-2862- fax: (0xx16) 602-2860.


