INTRODUCTIONNutritional implications of head and neck cancer are related to both the malignancy of the disease and the different interventions required to manage it.
The presence of cancer may lead to metabolic abnormalities, such as the increase in protein degradation, lyposis and production of glucose, as well as insulin resistance17. Secondary effects of antineoplasic treatment affect nutritional status. These effects may be acute or chronic and depend on location of tumor and irradiated region9.
Anorexia is a triggering or aggravating factor of protein-energy malnutrition. It occurs as a consequence of therapeutic treatments and/or systemic effects of the malignant tumor, and it may be intensified by the existence of infections, anxiety, chronic pain and possibly, chemical mediators12. Provision of nutritional therapy is important in each of the periods that involve the treatment of head and neck cancer (Figure 1).
Based on these aspects, we describe the repercussions of the disease and/or its treatment on the nutritional status of the patient and the importance of nutritional management as an additional component to the treatment of these patients.
Causes of protein-energy malnutrition
Nutritional care is essential in the treatment of head and neck cancer patients. Nutritional deficits are frequently seen even before medical intervention. They are a result of alcohol abuse and smoking, very common in these subjects35, and by the presence of tumor in the upper feeding tract, which leads to pain, edema, ulceration and bleeding and ends up interfering in mastication and swallowing of food16.
We should also consider the different types of surgical intervention to which patients are submitted, sometimes resulting in significant post-surgical implications, especially in malnourished elderly patients7. Radiotherapy of the head and neck reach normal tissues and cause complications such as xerostomia, mucositis, taste and olfaction abnormalities, food aversion, severe destruction of teeth and gums, dysphagia, odynophagia, muscle trismus, radiation dental cavities and chronic esophagitis8, 32. Anorexia is a common consequence of these complications. Therefore, depending on the feeding-related problems during radiotherapy, there is the need for dietary modifications according to complaints and detected limitations. This type of investigation should be constant, because the onset of symptoms may take place during the therapeutic treatment.
Nutritional problems occur even before radiotherapy treatment: dry mouth, taste changes, dysphagia and loss of appetite, in 25%, 14%, 40% and 20% of the patients, respectively. These symptoms increase considerably during the course of therapeutic treatment5, causing reduction of oral intake and affecting nutritional status. Taste changes are normally transient and there is total or partial recovery between 2 and 12 months after radiotherapy. However, some patients may experience permanent loss of taste28. Food aversion varies a lot and it is also transient, during the 1st and 3nd weeks of treatment. It involves one or more habitual food items and protein items (eggs, beef and dairy products), which are the most representative ones, requiring replacement by other protein sources20.
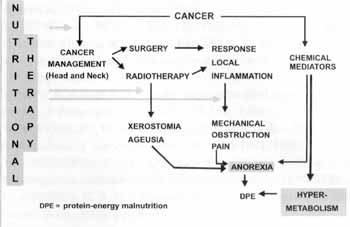
Figure 1. Nutritional implications of cancer and its treatment.
Beeken and Calman (1994)2 observed nutritional consequences one year after the end of curative treatment of oropharynx cancer and there was no resume of normal feeding pattern in all patients. Among them, the authors found that persistence of side effects to food adaptation and non-recovery of lost weight during treatment were present in 90% and 40% of the patients, respectively.
Since the existence of nutritional compromise is common even before proposed therapeutic treatment, and since it is an aggravating factor of malnutrition, we may preview that toxicity of treatment will prevent normal intake of nutrients during that period. This iatrogenic factor is a nutritional challenge that should be considered in the global treatment of these patients, and we should keep in mind that nutritional assessment if the first step of the treatment of protein-energy malnutrition. If done early, providing nutritional diagnosis preoperatively, there is also the possibility of identifying surgical risk patients22. This is an essential issue because the existence of malnutrition in a cancer patient impacts prognosis6.
Detection of protein-energy malnutrition
Assessment of food intake is part of the diagnosis of risk of protein-energy malnutrition, because energy intake has shown to be improper before and after radiotherapy of head and neck tumor5. Another simple and objective measure concerning nutritional state is the assessment of body weight, and it is common to observe weight loss before, during and after therapeutic treatment5. Weight loss seems to be related to site and size of irradiated area16. The use of anthropometric measures enables estimation of body composition, detecting the marasmatic form of protein-energy malnutrition characterized mainly by deletion of muscle tissue and subcutaneous fat, common in cancer patients. In a study in Brazil31, among 13 patients with head and neck tumors hospitalized for radiotherapy, we detected a deficit of arm muscle circumference in 7 patients pre-treatment, according to reference values. During treatment (2 weeks), muscle mass deficit decreased in 3 patients. Out of all anthropometric parameters assessed, there was predominant deficit of muscle mass, followed by deficits of body mass index and triceps cutaneous fold indicating energy reserve31.
Lab tests, such as the indicators of visceral proteins, contribute to the diagnosis of subclinical or marginal malnutrition, enabling intervention and prevention of nutritional problem at early stages.
The clinical use of immunological tests is minimal due to low specificity in the detection of protein-energy malnutrition, and immunosuppression observed in patients with head and neck tumors submitted to radiotherapy may be a result of the radiation that depresses the bone marrow, as well as radiosensitivity to lymphocytes T and B30. Another aspect to be observed is the use of chemotherapic agents, which are myelosuppressor drugs, also capable of affecting the function of bone marrow. Therefore, total lymphocyte count does not seem to be a good parameter to define the nutritional diagnosis of patients undergoing radiotherapy. Dias et al. (1996)8 concluded that conventional nutritional therapy did not prevent lymphopenia.
Finally, in order to diagnose correctly and shape proteinenergy malnutrition, we recommend that the nutritional classification be conducted by the combination of nutritional parameters3, since isolate nutritional parameters are inappropriate to determine the nutritional status of a subject.
Nutritionaltherapy
Indication of nutritional therapy should be based on previous, nutritional status of patient, type of tumor and specific interventions used in its treatment. The need for prolonged enteral supplementation is a consequence of factors such as: stage of disease, primary tumor in the pharyngeal region, preoperative loss of weight and aggressive treatment plan (surgery and radiotherapy)14. Whenever possible, we prefer oral feeding route; however, side effects of treatments sometimes hinder satisfactory food intake. In such cases, enteral nutrition; essential ac an early intervention measure. In our country. We detected the limited value of nutritional counseling as a way of solving the deficit of diet intake during radiotherapy, including protein-energy complementation of diet, which provided better nutrition to patients. Most probably, the intensity of anorexia observed in the 2nd week of radiotherapy was the factor that prevented the counseling to fulfill the nutritional needs of patients in the period31.
There are different methods of enteral nutrition available in the market, and each of them has advantages and disadvantages. The simplest and cheapest method is the use of nasogastric tube, and despite contraindicated in specific cases, it is used in patients who have been submitted to oropharyngeal surgeries29. Among the disadvantages of the use of nasogastric tube are nasopharyngeal ulceration, gastroesophageal reflux, disorder of healing of wounds and local mucositis. That is why its use should be avoided, especially in patients recovering from major surgeries29. Alternative route is enteral access via gastrostomy, frequently indicated in patients with head and neck tumor 27, especially endoscopic gastrostomy21. This type of technique is less invasive and similar to a surgical gastrostomy; however, it does not involve surgical procedure, sedation is minimal, visualization is direct, and the procedure is fast and cheap. The incidence of complications with endoscopic percutaneous gastrostomy is variable, from 10.5% to 35% of minor complications, and 0,7% to 22.5% of major complication33, 34, 37, 19, 26, 39. Minor complications described are dermatitis, ulcer, granulation tissue in the site of gastrostomy, leakage of gastric contents and formula, and dislocation of tube. Among major complications, we may list abdominal abscess, perforation/peritonitis, necrosis of stomach wall and intestine and pneumonia. Generally speaking, the technique is simple and safe, leading to few complications if performed by a specialized team39.
It is contraindicated in few conditions: hepatomegalia, ascites, and complications resulting from gastric resection27.
Gastrostomy is indicated if there is the need for nutritional therapy for a long period of time after the surgery (longer than 1 month), to replace the nasogastric tube14. Other factors that contribute to its indication are: presence of anatomical obstacles, mechanical or functional dysphagia, and patient's discomfort, hindering the use of nasogastric tube nutrition for a long period of time14, 27. Therefore, gastrostomy seems to be an effective alternative both for nasogastric tube 29 and administration of parenteral nutrition11.
Enteral nutrition may be combined to oral nutrition to provide transitory nutritional therapy, until the reduction of toxic effects of radiotherapy. Parenteral nutrition should be reserved to extreme cases and it seems little likely that it would benefit patients with advanced disease that do not respond to radio and/or chemotherapy36.
Indication of pre-op nutritional therapy is not common22, despite the existence of a relation between nutritional state and mortality and morbidity rates of patients. In addition to providing reduction in the incidence of post-op complications22, this kind of nutritional management results also in reduction of length of hospital stay13, essential to cut hospital costs11.
Early enteral nutrition in the post-op situation is equally important and as well-tolerated4 as pre-op nutritional intervention22. Moreover, nutritional modulation currently evidences the role of specific nutrients that seem to be essential for restoration and maintenance of cellular functions4.
Generally speaking, nutritional intervention undoubtedly reduces morbidity secondary to malnutrition and minimizes weight loss, as well as improves quality of life10. Oral supplementation showed increase in body weight and triceps cutaneous fold23, maintenance of albumin seric levels and more intake of total energy1. However, periodical supervision and rigid control of oral feeding are essential to meet the desired goals of nutritional therapy16. Hearne et al. (1985)16 studied patients with advanced head and neck cancer in radiotherapy treatment receiving enteral nutrition, and they confirmed higher energy and protein intake and less weight loss in patients with oropharynx and nasopharynx recurrent cancer. These data were compared to oral nutrition, which showed to be less effective than enteral, depending on the site of tumor. Another aspect of the use of enteral nutrition is its efficacy, similar to parenteral nutrition in maintaining or recovering nutritional status, in addition to being the most physiological route of administration; it reduced morbidity related to parenteral nutrition, maintains gastrointestinal structure and function and is easy to administer and has low cost's. Parenteral nutrition does not seem to be capable of reverting weight loss observed in cancer cachexia36. In addition, there is no evidence that it will benefit patients submitted to chemotherapy and radiotherapy, in terms of increase of response rate of tumor and/or prolongation of survival18.
In the event of nutritional intervention, there are controversial aspects as to improvement of response and tolerance to treatment, reduction of complications and prolonged survival. Evaluating some studies, Goodwin and Byers (1993)15 and Lopez et al. (1994)21 found better response and tolerance to treatment. Longer survival was observed by Lopez et al. (1994)21. Other studies reported absence of positive results concerning response and tolerance to treatment9, 36 and prognosis9, 24. Although these issues seem to be disagreeing according to the literature, malnutrition of head and neck cancer patients is very much related to deficit of intake, ratifying the importance of nutritional therapy39.
FINAL CONSIDERATIONSRadiotherapy of the head and neck results invariably in reduction of food intake. Negative energetic balance frequently persists for a period of time sufficient to aggravate or generate energetic deficit and, consequently, it may affect nutrient status (proteins, vitamins and minerals). Normally, weight loss is more marked when patients in radiotherapy are not submitted to prophylactic nutritional treatment. Therefore, for patients with some degree of protein-energy malnutrition the correct nutritional intervention would be adoption of early enteral nutrition associated with oral nutrition during intense radiotherapy.
In general, in the post-operative condition of head and neck surgery there is the need for enteral nutrition because the patient is enabled to feed himself normally. It is important to assess the appropriateness of nutritional intake (balance of food intake and nutritional needs), when oral intake is prescribed right after the surgery, considering the previous nutritional status of the subject and the surgery performed. In cases in which surgery is scheduled 7 to 10 days in advance, pre-op nutritional therapy may recover the reserves of glycogen, increase protein synthesis improving proteinemia and immunological status, and correct hydroimmunolytic deficits. History of fist weight loss before elective surgery may be important information, even if the patient weights more than his ideal weight.
In the indication of enteral nutrition, the choice of route of administration of diet relies on the estimated period of tube feeding, acceptance and comfort of patient. Situations that require tube feeding may be definite (obstruction caused mainly by neoplasia and permanent anorexia). Gastrostomy is a simple procedure that may be used via percutaneous access, using endoscopic and laparoscopic techniques. However, obstruction caused by tumor may hinder the passage of endoscope. The success of the procedure, with few complications, depends on the selection of techniques appropriate to each patient and specialized team.
By using gastric feeding through gastrostomy, two points favor nutritional provision: the use of larger tube and maintenance of the control of normal gastric emptying, with gradual release of food into the small intestine, improving digestion and absorption. Thus, the dietary provision has more energetic density and reduces the risk of obstructing the tube with foods and of gastrointestinal complications (osmotic diarrhea), especially in malnourished patients submitted to home nutritional therapy.
Prevalence of severe malnutrition is high in cases of squamous cell carcinomas of the head and neck because of the local effects of the tumor, poor feeding habits, syndrome of anorexia/cachexia induced by the tumor and the effects of radiotherapy and/or surgery. We know how difficult it is to restore nutrition completely, especially in cases of advanced cancer. In spite of that, nutritional treatment may maintain or recover, at some extent, the current nutritional status of patients, and reduce, therefore, the incidence of nutritional complications that may surge during post-op or radiotherapy. Because of these considerations, we propose a multidisciplinary preventive and therapeutic approach for management of patients with head and neck cancer.
REFERENCES1. ARNOLD, C.; RICHTER, M. P. -The effect of oral nutritional supplements on head and neck cancer. Int. J. Radiat. Oncol. Biol. Phys., 16: 1595-9, 1989.
2. BEEKEN, L.; CALMAN, F. -A return to "normal eating" after curative treatment for oral cancer. What are the long term prospects? Eur. J Cancer, 30: 387-92, 1994.
3. BLACKBURN, G. L.; HARVEY, K. B. - Nutritional assessment as a routine in clinical medicine. Postgrad. Med., 71:46-63, 1982.
4. BRAGA, M.; VIGNALI, A,.; GL4NOTTI, L.; CESTARI, A.; PROFILI, M.; CARLO, V. D. -Immune and nutritional effects of early enteral nutrition after major abdominal operations. Eur. J. Surg., 162: 105-12, 1996.
5. CHENCHARICK, J. D.; MOSSMAN, K. L. - Nutritional consequences of the radiotherapy of head and neck cancer. Cancer, 51: 811-5, 1983.
6. DALY, J. M.; REDMOND, H. P.; GALLAGHER, H. Perioperative nutrition in cancer patients. JPEN, 16: 100S-5S, 1992.
7. DI COSTANZO, J. - Role of preoperative nutritional status on postoperative morbidity. Ann. Fr. Anesth. Reanim., 14: Suppl.2, 33-8, 1995.
8. DIAS, M. C.; NADALIN, W.; BAXTER, Y. C.; FAINTUCH, J.; WAITZBERG, D.L.; MACULEVICIUS, J. - Acompanhamento nutricional de pacientes em radioterapia. Rev. Hosp. Clin. Fac. Med. Sao Paulo, 51: 53-9, 1996.
9. DONALDSON, S. S. - Nutritional support as an adjunct to radiation therapy. JPEN, 8: 302-10, 1984.
10. DWYER, J. T.; EFSTATHION, A.; PALMER, C.; PAPAS, A. Nutritional support in treatment of oral carcinomas. Nutr. Rev., 49: 332-7, 1991.
11. ELLIS, L. M.; COPELAND, E. M.; SOUBA, W. W.- Perioperative nutritional support. Surg. Clin. North Am., 71: 493-507, 1991.
12. FANELLI, F. R.; LAVIANO, A.; MUSCARITOLI, M.; PREZIOSA, L; ARIEMMA, S.; CANGIANO, C. - Anorexia associated to chronic illnesses: new pathogenic and therapeutic insights. Rev. Bras. Nutr. Clin., 10: 101-6, 1995.
13. FLYNN, M. B.; LEIGHTTY, F. F. - Preoperative outpatient nutritional support of patients with squamous cancer of the upper aerodigestive tract. Am. J. Surg., 154: 359-62, 1987.
14. GARDINE, R. L.; KOKAL, W. A.; BEATTY, J. D.; RIIHIMAKI, D. U.; WAGMAN, L. D.; TERZ, J. J. - Predicting the need for prolonged enteral supplementation in the patient with head and neck cancer. Am. J. Surg., 156- 63-5, 1988.
15. GOODWIN W. J. Jr.; BYERS, P. M. -Nutritional management of the head and neck cancer patient. Med. Clin. North Am., 77: 597-610, 1993.
16. HEARNE, B. E.; DUNAJ, J. M.; DALY, J. M.; STRONG, E. W.; VIKRAM, B.; LePORTE, B. J.; DeCOSSE, J. J. - Enteral nutrition support in head and neck cancer: tube vs. oral feeding during radiation therapy. J. Am. Diet. Assoc., 85: 669-74, 677, 1985.
17. HEBER, D.; TCHEKMEDYIAN, N. S. - Pathophysiology of cancer: hormonal and metabolic abnormalities. Oncology, 49: Suppl.2, 28-31, 1992.
18. HEYS, S. D.; PARK, K.G.; GARLICK, P. J.; EREMIN, O. Nutrition and malignant disease: implications for surgical practice. Br. J. Surg., 79: 614-23, 1992.
19. HOFFER, E. K.; COSGROVE, J. M.; LEVIN, D. Q.; HERSKOWITZ, M. M.; SCLAFANI, S. J. - Radiologic gastrojejunostomy and percutaneous endoscopic gastrostomy: a prospective, randomized comparison. J. Vasc. Intern. Radiol., 10:413-20, 1999.
20. JACOBSEN, P. B.; SCHWARTZ, M. D. -Food aversions during icancertherapy: incidence, etiology, and prevention. Oncology, 7.-(Suppl), 139-43, 1993.
21. LOPEZ, M. J.; ROBINSON, P.; MADDEN, T.; HIGHBARGER, T. -Nutritional support and prognosis in patients with head and neck cancer. J. Surg. Oncol., 55: 33-6, 1994.
22. MEIJERINK, W. J. H. J.; VON MEYENFELDT, M. F.; ROUFLART, M. M. J.; SOETERS, P. B. Efficacy of perioperative nutritional support. Lancet, 340: 187-8, 1992.
23. NAYEL, H.; GHONEIMY, E.; HADDAD, S. - Impact of nutritional supplementation on treatment delay and morbidity in patients with head and neck tumors treated with irradiation. Nutrition, 8: 13-8, 1992.
24. PEZNER, R. D.; ARCHAMBEAU, J. O.; LIPSETT. J. A.; KOKAL, W. A.; THAYER, W.; HILL, L. R. -Tube feeding enteral nutritional support in patients receiving radiation therapy for advanced head and neck cancer. Int. J. Radiat. Oncol. Biol. Phys., 13:
935-9, 1987.
25. RASSLAN, S.; PONZONI, M.E.; BIROLINI, C. - Nutrição parenteral pre-operat6ria no doente corn cancer. Acta Oneol. Bras., 12: 14-8, 1992.
26. RAYNOR, E. M.; WILLIAMS, M. F.; MARTINDALE, R. G.; PORUBSKY, E. S. - Timing of percutaneous endoscopic gastrostomy tube placement in head and neck cancer patients. Otolaryngol. Head Neck Surg., 120: 479-82, 1999.
27. RIGHI, D.; GARRETTI, L.; ZANON, E.; GAZZERA, C.; CRISTOFERI, M.; GANDINI, G. - Percutaneous gastrostomy. Personal experience in 137 cases. Radiol. Med. Torino, 88: 789-92, 1994.
28. RITCHIE, J. R.; BROWN, J. R.; GUERRA, L. R.; MASON, G. - Dental care for the irradiated cancer patient. Quit. Int., 12: 837-41, 1985.
29. ROUKEMA, J. A.; VAN DER WERKEN, C.; JUTTMANN, J. R. - Percutaneous endoscopic gastrostomy as a standard procedure in head and neck surgery. Arch. Otolaryngol. Head Neck Surg., 116 730-1, 1990.
30. SAVINA, N. P.; MEDVEDEV, V. S.; KUZINA, A. A. -Effect of contact neutron and gamma therapy on immunity of patients with cancer of the mouth mucosa. Med. Radiol. Mosk, 31: 138, 1986.
31. SBAN. IV Congresso Nacional da Sociedade Brasileira de Alimentação a Nutrição. Nutrição a qualidade de vida. Livro de resumos. p.103, 1996.
32. SILVAIN, C.; BARRIOZ, T.; BESSON; I.; BABIN, P.; FONTANEL, J. P.; DABAN, A.; MATUCHANSKY, C.; BEAUCHANT, M. Treatment and long-term outcome of chronic radiation esophagitis after radiation therapy for head and neck tumors. Dig. Dis. Sci., 38: 927-31, 1993.
33. SO, J. B. Y.; ACKROYD, F. W. -Experience of percutaneous endoscopic gastrostomy at Massachusetts General Hospital: indications and complications. S. M. J. 39: 560-3. 1998.
34. TALLER, A.; HORVATH, E.; HARSANYI, L.; KOTAI, Z.; SIMIG, M.; ILIAS, L. - Percutaneous endoscopic gastrostomy: 3 years experiences. Orvosi Hetilap., 140: 1347-52, 1999.
35. THOMAS, D. B. - Alcohol as a cause of cancer. Environ. Health Perspect., 103: Suppl 8, 153-60, 1995.
36. TISDALE, M. J. - Cancer cachexia. Anti-Cancer Drugs, 4: 115-25, 1993.
37. WALTON, G. M. - Complications of percutaneous gastrostomy in patients with head and neck cancer-an analysis of 42 consecutive patients. Ann. R. Coll. Surg. Engl., 81: 272-
6, 1999.
38. YAKOUN, M. - In which patients has the efficacy of preoperative artificial nutrition be proved? Ann. Fr. Anesth. Reanim., 14: Suppl. 2, 47-53, 1995.
39. ZENK, J.; WALDFAHRER, F.; PETSCH, S.; IRO, H. - Long-term experience with percutaneous endoscopic controlled gastrostomy (PEG) in ENT tumor patients. HNO, 46: 660-5,1998.
* Nutritionist with Centro de Metabolismo a Nutrição (CeMeNutri) at Faculdade de Medicina da Universidade Estadual Paulista - UNESP - Botucatu/ SP. Master in Metabolism and Nutrition at UNESP - Botucatu/ SP.
** Professor of the Department of Otorhinolaryngology at Faculdade de Medicina da Universidade Estadual Paulista de Botucatu/ SP - Discipline of Head and Neck Surgery. Master in General Basis Surgery and Experimental Surgery at Universidade Estadual Paulista - UNESP - Botucatu/ SP.
*** Centro de Metabolismo a Nutrição (CeMeNutri) da Faculdade de Medicina da UNESP - Botucatu/ SP. Faculty Professor of the Department of Clinical Medicine at Faculdade de Medicina da UNESP - Botucatu/ SP.
Address for correspondence: Roberto C. Burini - Centro de Metabolismo a Nutrição (CeMeNutri), Distrito de Rubião Junior - 18618-000 Botucatu/ SP.
Fax: (55 14) 822-2238.
Article submitted on August 27, 2000. Article accepted on August 31, 2000.


