INTRODUCTIONChronic renal failure is a syndrome resultant from various etiologies, such as interstitial, glomerular, hereditary, obstructive and vascular renal diseases2. The main diseases associated with chronic renal failure (CRF) are systemic arterial hypertension, diabetes mellitus and glomerulonephritis3.
CRF has a progressive and insidious evolution, divided in 4 stages2: reduced renal reserve (rate of glomerular filtration in about 50/0 of normal), renal failure (filtration between 20 to 50% of normal), renal severe failure (filtration lower than 20% of normal) and terminal renal disease (filtration below 5% of normal).
The diagnosis of chronic renal failure is based on documentation of elevated seric levels of creatinine and/or urea for a long time, anemia, radiological imaging of kidneys smaller in volume, and presence of osteodystrophy in x-rays4. Treatment, at first conservative, aims at controlling symptoms and minimizing complications, as well as delaying the progression of the disease, which may be obtained by reverting the triggering causes and using specific dietary and drug techniques: Treatment with hemodialysis and renal transplant is reserved to unsuccessful cases of conservative treatment, normally present in advanced stages4.
The fact that the cochlea is susceptible to a wide variety of metabolic, hydroelectrolytic and hormonal imbalances is already widely known and these imbalances are systemic alterations usually found in patients who have compromised renal function. Therefore, it is expected that subjects with CRF develop cochlear dysfunction, clinically manifested by sensorineural hearing loss.
Hutchinson10 observed in his study the existence of a direct relation between CRF and sensorineural hearing loss.
Oda15 described histological alterations of temporal bones in renal patients in hemodialysis and/or post-transplant', suggesting the existence of damage to Corti's organ cochlear cells.
Hutchinson10 found a high prevalence of sensorineural hearing loss in high frequencies in pure tone audiometry of CRF patients. However, he did not observe alterations of the speech recognition index10. On the other hand, Isselbacher11, Kligerman12 and Mancini13 reported hearing losses with significant clinical impact.
Nikopoulos14, Oda15 and Shvili16 observed alterations of evoked brainstem potentials in chronic renal patients, such as increase in latency of waves III and IV, suggesting the existence of neural lesions, in addition to sensorial ones (uremic neuropathy).
Nevertheless, the direct relation between CRF and sensorineural hearing loss is not unanimously considered by the literature. Some authors such as Mancini13 and Gafter6 disagree that CRF would be a etiological factor of sensorineural hearing loss.
The objectives of the present study were: 1) to check the difference between minimal audible thresholds of normal subjects and patients with chronic renal failure; 2) observe the influence of hemodialysis in minimal audible thresholds; 3) investigate if chronic renal failure may be considered the direct cause of sensorineural hearing loss, and 4) evaluate the value of audiometry in the diagnosis of hearing loss in patients with CRF.
MATERIAL AND METHODThe population we studied included subjects aged 15 to 60 years who had renal failure in the stages of failure, severe failure or terminal renal disease, that is to say, patients who had more than 40% to 50% of the renal function compromised. Sixteen patients with renal failure submitted to conservative treatment formed group A, 17 patients with renal failure submitted to hemodialysis were group B and 16 other subjects of the same age range and without renal pathology or hearing cor4plaints were the control group (group C). Age limits were defined aimed at having a homogenous and normal hearing population from a scientific point of view9.
We excluded subjects who had history of hearing loss previous to CRF, risk of occupational otological disease (exposure to noise or solvent), diabetes mellitus or other metabolic diseases, Alport syndrome or family history of primary low hearing disability, external or middle ear pathologies at physical exam, air-bone gap in audiometry, tympanometric curves types B or C7, 9, 10, 13. We also excluded patients who had taken aminoglycoside antibiotics for more than 7 days or that were using furosemide in doses higher than lmg/Kg/day13.
The candidates for the study were referred by the nephrology department of Hospital de Clínicas da UFPR, and the diagnosis of CRF was confirmed by the records in the medical files, according to the criteria already presented in the introduction of this article, especially creatinine clearance values lower than 60ml/min/1.73m² for more than 3 months11. These subjects were submitted to anamnesis, ENT exam and pure tone audiometry, followed by speech recognition index in order to check their eligibility for the study. Data were recorded in standardized protocols that comprised the analyzed material.
Acoustic immitanciometry included static and dynamic complacency and acoustic stapedial reflex, and it was performed in all subjects. The exam was conducted in order to exclude middle ear pathologies at subclinical stages and to detect the presence of recruitment, a known indicative of corticopathy.
Statistical analysis included the study of the differences in mean threshold values for each group using t Student's test. The study was conducted with a confidence interval of 95%.
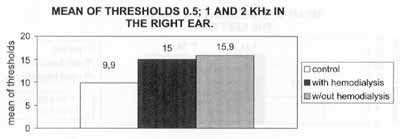
Graph 1. Mean of auditory thresholds of 0,5; 1 and 2 KHz in the right ear.
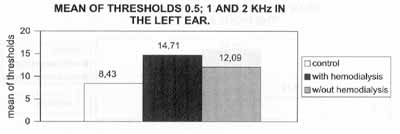
Graph 2. Mean of auditory thresholds of 0,5; 1 and 2 KHz in the left ear.
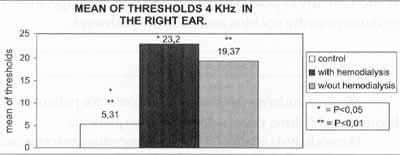
Graph 3. Mean of auditory thresholds of 4 KHz in the right ear.
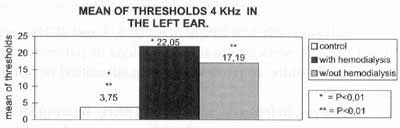
Graph 4. Mean of auditory thresholds of 4 KHz in the left ear.
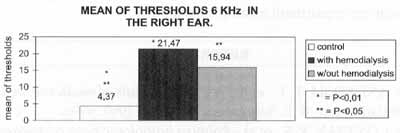
Graph 5. Mean of auditory thresholds of 6 KHz in the right ear.
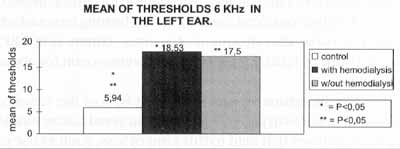
Graph 6. Mean of auditory thresholds of 6 KHz in the left ear.
This study was appreciated and approved by the Committee of Ethics for Research in Human Beings at Hospital de Clínicas da Universidade Federal do Parana.
RESULTSThe mean ages of patients in group A was 33.69 ± 10.45 years; in group B it was 36.65 ± 10.63 years; and in control group C, it was 44.94 ± 11.72 years. These results did not present statistically significant difference. Means for creatinine clearance were: 32.64 t 13.64; 14.59 ±11.58; and 117.94 t 13.23 respectively.
Means of auditory thresholds for 0.5, 1 and 2 KHz were 15.9;15 and 9.9 (in right ear) and 12.09;14.71; and 8.43 (in left ear) - respectively. These results did not show statistically significant difference.
Means of auditory thresholds for 4 KHz were .19,37; 23.23 and 5.31 (in right ear) and 17.19, 22.05 and 3.75 (in left ear) - for groups A, B and C, respectively. We observed statistically significant difference when comparing the control group and the studied groups, but not between the studied groups. These results were similar to those obtained, in the frequency 6 KHz, as we may see in the Graphs presented here.
The mean auditory thresholds in 8 KHz were 16.9, 25.88 and 8.12 (in right ear) and 24.06; 24.12 and 9.35 (in left ear) for groups A, B and C, respectively. In the right ear, we had a difference between the control group and group B, but not between the control group and group A. In the left side, there was statistically significant difference between control group C, and studied groups (A and B), but not between the groups themselves.
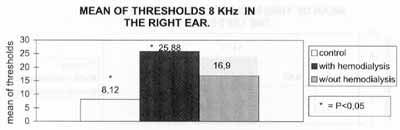
Graph 7. Mean of auditory thresholds of 8 KHz in the right ear.
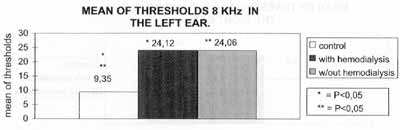
Graph 8. Mean of auditory thresholds of 8 KHz in the left ear.
Analyzing only low frequencies (0.5, 1 and 2KHz), we did not observe sensorineural hearing loss in patients with chronic renal failure, regardless of being submitted or not to hemodialysis.
However, in frequencies 4, 6, and 8KHz hearing levels of renal patients were statistically different from the control group, showing mild sensorineural hearing losses. In these frequencies, the result was similar to that reported by Kligerman et al.12, who found a large incidence of hearing losses in high frequencies. Gatland7 and Nikolopoulos14 obtained results that showed sensorineural deficits with significant clinical impact. Facharzt4 found considerable sensorineural hearing losses which were reversible after treatment of anemia (common in CRF) using a dose of 120U/Kg per weeks of erytropoetin for about 6 months.
The literature reports that about 80% of the cases of sensorineural loss in patients with chronic renal failure would be due to causes that lead to this kind of loss, such as use of aminoglycosides, or occupational exposure to noise10, 13. The remaining 20% would be directly caused by CRF. However, because of its complex clinical condition, demanding the use of various drugs, with multiple etiologies and affecting especially the elderly, it is difficult to investigate its correlation with hearing acuity. This explains the controversy in the area.
Based on the results, it is suggested that there is a direct relation of CRF as the cause of sensorineural hearing loss, especially in high frequencies.
Considering the absence of statistically significant difference between the group with CRF and hemodialysis and the group submitted to conservative treatment, we may state that hemodialysis is not directly related with hearing loss, a fact supported by other studies reported here.
In fact, since hemodialysis corrects a large part of hydroelectric and metabolic disorders, it tends to reduce the risks of hearing loss, because it promotes stabilization and correction of metabolic alterations caused by chronic renal failure. Therefore, the correct treatment for CRF should be initiated as early as possible, preventing body damage, including damage to the cochlea and auditory pathways.
CONCLUSIONSMinimal auditory thresholds were lower for patients with chronic renal failure, especially in high frequencies.
Hemodialysis is not a factor that generates sensorineural hewing loss in chronic renal patients submitted to dialytic treatment.
We observed a direct relation between chronic renal failure and sensorineural hearing loss in high frequencies.
Audiometry proved to be a reliable test for diagnosis of hearing impairment in subjects with CRF.
REFERENCES1. ANDREOLI, T. E., et al. - Cecil essentials of medicine. 4ed. Philadelphia: W.B. Saunders Company, 1997. 999p.
2. CONTRAN, R. S., et al. - Robbins patbologic basis of disease. 5 ed. Philadelphia: W.B. Saunders Company, 1997. 999p.
3. ENCONTRO BRASILEIRO DE TRABALHOS CIENTIFICOS EM OTORRINOLARINGOLOGIA (3:1997: Rio de Janeiro) Anais. Rio de Janeiro: JZ promoções, 1997
4. FACHARZT, F. A. et al. - Reversible uremic deafness: is it correlated with the degree of anemia? Ann. Otol. Rbinol. Laryngol., 106, 391-393, 1997.
5. GAFTER, U., et al. Brainstem Auditory Evoked Responses in Chronic Renal Failure and the Effect of Hemodialysis. Nepbron, 53 (2-5), 1-5, 1989.
6. GAFTER, U., et al. - Brainstem Auditory Evoked Responses in Chronic Renal Failurc0and the Effect of Hemodialysis. Brainstem auditory evoked potentials in chronic renal failure and maintenance hemodialysis. Neurology, 35, 419-423, 1985.
7. GATLAND. D. et al. Hearing loss in chronic renal failure hearing threshold changes following haemodialysis. J. R. Soc. Med., 84(2), 587-589, 1991.
8. GILMANN, A. G. - Goodman a Gilman: as bases farmacologicasda terapeutica.8a. ed. Rio de Janeiro: Guanabara Koogan, 1991.1232p.
9. HUNGRIA, H. - Otorrinolaringologia. 7ª. ed. Rio de Janeiro: Guanabara Koogan, 1995. 489p.
10. HUTCHINSON, J. C., et al. - Electrophysiologic Analysis of Auditory, Vestibular and Brain Stem Function in Chronic Renal Failure. Laryngoscope, 92, 833-843, 1982.
11. ISSELBACHER, K. - Medicinalnterna.13ª. ed. Nueva Editorial Interamericana: Mexico, 1995. 2622p.
12. KLIGERMAN, A. B. et al. - Hearing Impairment Associated with Chronic Renal Failure. Laryngoscope, 91, 583-592, 1981.
13. MANCINI, M.L. et al. - Sensorial hearing loss in patients reaching chronic renal failure in childhood. Pediatr. Nephrol., 10. 38-40, 1996.
14. NIKOLOPOULOS, T. P., et al. -Auditory function in young patients with chronic renal failure. Clin. Otolaryngol., 22(3), 222-225,1997.
15. ODA, M. et al. - Labyrinthine pathology of chronic renal failure patients with hemodialysis and kidney transplantation. Laryngoscope, 84, 1489-1506, 1974.
16. SHVILI, Y. et al. - Brainstem auditory evoked responses in rats with experimental chronic renal failure. Clinical Science, 76, 415-417, 1989.
17. TIERNEY, L. M. et al. - Current medical diagnosis treatment. 36 ed. London: Appleton & Lange, 1997. 1587p.
* Physician of the Service of Otorhinolaryngology at Hospital de Clínicas da Universidade Federal do Paraná - UFPR.
** Faculty Professor and Head of the Service of Otorhinolaryngologist at Hospital de Clínicas da UFPR.
*** Physician of the Service of Otorhinolaryngology at Hospital de Clínicas da UFPR.
**** Resident Physician of the Service of Otorhinolaryngology at Hospital de Clínicas da UFPR.
***** Speech and Hearing Pathologist of the Service of Otorhinolaryngology at Hospital de Clínicas da UFPR.
Department of Otorhinolaryngology and Ophthalmology at Hospital de Clínicas da UFPR.
Address for correspondence: Guilherme L. Trevizan - Rua Menezes Dória, 184 - Hugo Lange - 80040-350 Curitiba/ PR - Tel/Fax: (55 41) 254-2767.
Article submitted on August 11, 2000. Article accepted on September 28, 2000.


