INTRODUCTIONPapanicolaou, in 1943, created the method of cytodiagnosis for prevention of cancer of female genital system, investigating desquamated cells of vaginal mucosa to determine the effects of sexual hormones on the epithelium and, therefore, identify desquamated neoplasic cells in the smears10.
The test we conducted in the present study was exfoliate cytology, based on the possibility of analyzing cells from the epithelial surface that are physiologically desquamated, due to the continuous process of renovation of basal layer8. This simple and affordable method, if performed periodically, can detect pre-neoplasic lesions and some infections and control extensive leukoplasia that may not be removed - it enables identification of initial microscopic alterations, and therefore, tracking of high risk population of patients8.
Silverman, Bilimoria, Bhargava, Mani and Shah (1977)13 stated that precision of exfoliate cytology increased when used to analyze lesions before biopsy in high risk adult populations. Since the oral epithelium is constantly renovated (every two weeks), and most of epithelial cells contain a nucleus, superficial and direct smear may be a reliable indicator of displasic or neoplasic alterations, producing a safe sample of lesion and helping complete tracking. Early detection by cytological tracking may speed up diagnosis and treatment, reducing morbidity and mortality. The main use of cytology for detection of oral cancer is justified by the fact that 95% of all malignant neoplasia are from epithelial origin; many studies stated that the use of exfoliate cytology has sped up the indication of biopsy of lesions that clinically did not seem to be malignant. It has led to early diagnosis of oral lesions that remained unsuspected for some time, then confirmed through incision or excision biopsy.
There are many lesions that affect the lips, among them chronic irritations, such as leukoplasia, erytroplasia, lip inflammation and carcinoma. The irritations may arise from mechanical trauma, solar radiation and chemical substances such as tobacco. In addition, we should bear in mind that in many situations oral cancer is preceded by cancerous states of the mucosa; such states may be present in a number of cases with prolonged progression, considering that health is integrated with the environment and the actions of humans beings over it3.
It is known that lower lip vermilion border becomes dried as a result of sun, wind or frost exposure, leading to hyperkeratotic alterations, from where most of malignant lesions are originated. For this reason, people that work exposed to sun and weathered conditions (fishermen, sailors and agriculture workers, among others), especially those who have thin and little pigmented skin, consist of the majority of patients affected by this kind of pathology14.
The first risk factor of lip cancer is actinic data, and in many cases squamous cells of lip carcinoma develop in areas in which there had already been acute or chronic actinic lip inflammation: The acute form is manifested with superficial inflammation and occasional blisters, whereas the chronic manifestation presents vertical striae, perpendicular to the skin and the vermilion border, hyperkeratosis, erythema, and a thick area underneath the lip skin. Lip cancer is ulcerated, presenting abnormal growth, with blisters and exophilic lesions and it may transform an area of inflammation into a displasic area. Verrucous alterations, erythema, hyperkeratosis, and non-healing lesions are indications of malignancy, which should be carefully examined through biopsy, because cytology and regular staining do not confirm the diagnosis of lip cancer1. Lower lip mucosa is especially susceptible to actinic damage, which seems to be the main cause of cancer in the region2.
Tobacco may lead to mechanical damage, caused by the friction of the cigarette or pipe against lip epithelium during smoking, thermal damage because of the heat that is transmitted to the lip epithelium, and chemical damage because there are more than 4,720 substances in tobacco found to be potential cancerous, such as hydrocarbons, volatile nitrosamines, nickel, arsenic, and phenols, to name, but a few3. In such cases, in addition to chemical damage caused by combustion products of tobacco, and physical damage caused by heat, there is mechanical and physical irritation caused by chronic friction, especially because the lips are in constant movement14.
Non-keratinized squamous epithelium may form keratin because of various circumstances and especially due to the influence of chronic irritation.
The responses of oral mucosa to physical, chemical or biological agents vary a lot when it comes to clinical presentation. Smears of these lesions may reveal paranasal cells with enlarged nucleus and little cytoplasm around, followed by multiple and prominent nucleoli, abnormal chromatic aspects and multi-nucleated cells. These alterations demonstrate that cells are of suspicion and displasic appearance, showing the importance of clinical correlation and microscopic findings to determine a rational intervention of prevention and control of patients submitted to the action of these agents12.
A hypothesis accepted currently is that more than 80% of human malignant neoplasia are directly or indirectly related to extrinsic or environmental factors, which means that many of them could be prevented14.
Early diagnosis has favored treatment in most of the patients with this affection6,7. In addition, early diagnosis of oral tumors should not be of great difficulty, since the risk group is well characterized, and the region is of easy access for clinical exam. The main point to have in mind is the possibility of diagnosis, especially in high risk patients.
Owing to the scarcity of Brazilian literature available about the topic, this pilot study intended to investigate alterations of lower lip vermilion border by exfoliate cytology in subjects submitted to sun exposure and smoking, comparing them to control subjects without exposure, defining risk groups that should be watched for prevention and early diagnosis of cancer.
MATERIAL AND METHODThree hundred and twenty two smear slides from 161 patients (2 smears each) were analyzed at the Service of Cytology in the Department of Pathologic Anatomy at Santa Casa de Misericórdia de São Paulo. There were 100 men and 61 women, mean age of 41.6 years. They were divided into 4 groups, as follows:
Group 1: formed by 54 control patients (33.54%), non-exposed to sun radiation (working indoors) and non-smokers.
Group II: formed by 43 patients exposed to sun radiation (26.71%) and non-smokers, with an average of 19 years of sun exposure. This group was divided into 2 subgroups: the first one, with 16 patients, continuously exposed (8 to 10 hours a day), and the second group, with 27 patients submitted to intermittent exposure (duration of exposure was not quantified).
Group III: formed by 36 smoking patients (22.71%), all of them smoked different commercial brands of cigarettes with filter, and they had been smoking for at least 10 years and smoked 10 to 30 cigarettes a day.
Group IV: formed by 28 patients (17.39%), who smoked and had sun exposure.
All patients answered a detailed questionnaire (Figure 1) containing name, age, sex, race, profession, smoking habit (daily quantity and duration of habit), sun exposure (daily exposure and duration of exposure).
Two smears from each patient were obtained using exfoliate cytology of lip semi-mucosa, and the areas from which the samples were collected were clinically normal.
All slides were analyzed with optic microscopy; using binocular microscopy and following Papanicolaou battery:
o Harris Hematoxylin (stains leukocytes, basophilic nucleus and cytoplasm);
o Orange (stains keratinized cells, acidophilic cytoplasm and red blood cells);
o EA - eosin (stains acidophilic elements) light green (stains basophilic elements) and vesuvin (color shades).
We carried out a qualitative cytological assessment (observation of cell alterations, such as enlargement of nucleus size, enlarged nucleoli, nuclear hyperchromatism, cellular multinucleation and cellular keratinization), and a quantitative one (count of cells with different degrees of exfoliate maturation of oral mucosa) (Figure 2). The statistical test used was Kruskal Wallis, for comparison of control, sun exposure, sun exposure + smoking, and smoking groups. We considered the statistically significant difference p < 0.05.
Figure 1. Questionnaire for patients to answer.
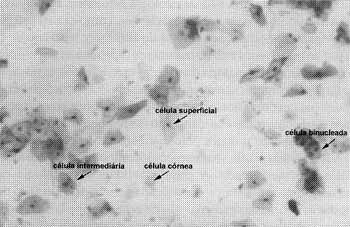
Figure 2. Cells of stratified pavement epithelium of lower lip, 200xA.0. Papanicolaou staining.
Based on the averages obtained, we found an increase in keratin layer (keratinized cells) in cases of surf exposure and smoking, and in the group of both smoking and sun exposure the incidence was even higher. We obtained 27.53% in relation with the control group (22.20%) (Table 1).
Table 1 shows that in the group of smokers (group 3) we found 57.69% of intermediary cells against 56.35% in the control group. The percentage of binucleated cells (1.04%) in smokers, smokers was also higher than in the control group (0.84%), but there was no statistically significant difference.
TABLE 1 - Average of detected cells.
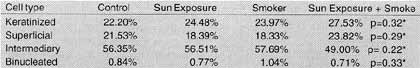
* Test Kruskal Wallis, to compare groups: control, sun exposure, smoker, sun exposure + smokers.
Vermilion border mucosa is named semi-mucosa because it is the intermediary layer between the non-keratinized oral mucosa and the skin, presenting a thin layer of keratin, as seen in the results of the control group.
In the groups with chronic irritation caused by smoking and sun exposure, the layer of keratin is thicker determining an increase in number of keratinized cells and showing the cytological alterations of the mucosa5, 13.14.
The largest number of cells was present in, patients with sun exposure combined with smoking (27.53% against 22.20% in control group), because they had suffered an aggression against the epithelium, due to heat and traumatism.
Secondly, there were the patients with sun exposure (24.48%), and in third place, the smokers (23.97%).
In the group of smoker patients (group 3), we noticed two significant alterations compared to the other groups:
a) increase in layer of intermediary cells (57.69% against 56.35% from the control group), and
b) increase in number of binucleated cells (1.04% against 0.84% from the control group).
Therefore, we concluded that the mechanical damage caused by cigarette to the lip epithelium causes the enlargement of the cell layer, showing tissue suffering with hypertrophy and hyperplasia of intermediary layers (prickle cells)4,9 with a slight increase in number of binucleated cells, common findings in normal smears. The response of oral mucosa to physical, chemical or biological agents vary a lot in clinical appearance. Smears of these lesions may reveal paranasal cells with enlarged nucleus and little cytoplasm around, surging sometimes multiple and prominent nucleoli, abnormal chromatic aspects and multi-nucleated cells6.
The finding of increased number of binucleated cells in the smoker group (group 3) compared to the others groups made us believe that physical damage (heat), chemical damage (cigarette substances) and mechanical damage (friction) caused by the use of tobacco had triggered it.
The same reaction is not found in the group with sun exposure, in the group with both sun exposure and smoking, and in the control group. We may conclude that the reaction of the mucosa to smoking is different from the reaction to sun exposure, even if both exposures are present. We concluded that smokers have an increase in cellular binucleation, and smokers exposure to sun have an increase in keratinized cells (hyperkeratosis), without increase in binucleated cells. Maybe the onset of hyperkeratosis is earlier, protecting deeper layers and avoiding binucleation.
Both alterations are, in our opinion, demonstrations of tissue reaction to irritation factors, with displasic alterations that could predispose to carcinoma progression if damage persists. We also supposed that there is a synergetic effect between smoking and sun exposure in the genesis of hyperkeratosis, known as pre-cancer lesions, and we may also state that the most common histologic alteration in lip cancer is epithelial hyperplasia, observed in 80% of the cases11.
We did not find significant alterations at exfoliate cytology in cases of sun exposure only. Maybe it is due to the fact that most of our population consisted of people of darker skin, less sensitive to sun irritation than those coming from the north hemisphere, who usually have lighter skin. These alterations occur even before the lesions present clinical manifestations, and that is why we suggest further investigation in this group of patients, correlating the findings of pre-neoplasic and neoplasic lesions.
CONCLUSIONTo summarize, we may conclude that smoking associated with sun exposure cause cytological alterations in the epithelium of lip semi-mucosa even before it becomes a clinically visible lesion. If the irritation persists, these alterations indicate the surge of pre-neoplasic and neoplasic lesions, and the population may be considered as risk group. Moreover, exfoliate cytology is a simple and economical method, and it may be used as routine in risk populations, aiming at primary prevention of lower lip cancer.
REFERENCES1. AWDE, J. D.; KOGON, S. L.; MORIN. R. J. - Lip Cancer: A Review. J. Can. Dent. Assoc., 62: 634-636, 1996.
2. CAWSON, R. A.; BINNIE, W. H.; EVERSON, J. W. - Atlas colorido. 2 ed. São Paulo: Artes Médicas, 1997.
3. GENOVESE, W. J. - Câncer de boca. Noções básicas para prevenção a diagnóstico. São Paulo: Fundação Peirópolis, 1997.
4. JUNQUEIRA, L. C.; CARNEIRO, J. - Histologia básica. 8 ed. Rio de Janeiro: Guanabara,1995.
5. KOSS, L. G. - Diagnostic cytology and its bistopatbologic bases. 3 ed. Philadelphia: Lippincott, 1979.
6. KOWALSKY, L. P. - Carcinoma da boca: epidemiologia, diagnóstico a tratamento. Acta AWHO, 10: 128-131, 1991.
7. MENDONCA. C. A. B.: KLIGERMAN, J.; MEDEIROS, F. A. O. - Câncer do Lábio Inferior. Rev. Bras. de Cancerol., 29: 2-6, 1983.
8. MONTENEGRO, M. R. - Patologia-processos gerais. 3 ed. São Paulo: Atheneu; 1992.
9. NIEBURGS, H. E. - Diagnostic cell patbology in tissue and smears. New York: Grune & Stratton, 1967.
10. PAPANICOLAOU, G. N. - Atlas of Exfoliative Cytology. Cambridge: Harvard University Press, 1993.
11. SHARMA, P. K.; SCHULLER, D. E.; BEKER, S. R. -Malignant Neoplasms of the Oral Cavity. In: CUMMINGS, C. W. et al. Otolaryngology Head & Neck Surgery. 3 ed. St. Louis: Mosby Year Book Inc., 1998.
12. SILVERMAN Jr., S. - Oral cavity. In: BIBBO, M. D. Comprehensive cytopathology. Philadelphia: Saunders, 1991.
13. SILVERMAN Jr., S.; BILIMORIA, K. F.; BHARGAVA, K.; MANI, N. J.; SHAH, R. A. - Cytological, Histologic and Clinical Correlations of Precancerous and Cancerous Oral Lesions in 57, 518 Industrial Workers of Gujarat, India. Acta Cytol., 21: 196-198, 1977.
14. TOMMASI, A. F.; GARRAFA, V. - Câncer Bucal. São Paulo: Medisa Editora Ltda., 1980.
* Master Degree In Head and Neck Surgery, Hospital Heliópolis/ SP.
** Surgeon of the Service of Head and Neck Surgery, Hospital Heliópolis/ SP.
*** Head of the Service of Oral Semiology of Instituto Arnaldo Vieira de Carvalho/ SP.
**** Pathologist of the Department of Pathologic Anatomy at Faculdade de Ciências Médicas de São Paulo /SP.
***** Coordinator of Post-Graduation Course- Hospital Heliópolis /SP.
Address for correspondence: Prof. Dr. Jozias de Andrade Sobrinho - Curso de Pós-Graduação em Cirurgia de Cabeça a Pescoço do Hospital Heliópolis/ SP
Rua Cônego Xavier, 276 - 10° andar - 04231-020 São Paulo/ SP - Tel/fax: (55 11) 273-9016
E-mail: cpgcp.hosphel@ibm.net
Article submitted on May 22, 2000. Article accepted on July 13, 2000.


