INTRODUCTIONThe relation between nasal pathology and asthma and has been described for centuries. Galenus in second century, believed that secretions in nasal fossa and lower airways were originated from the brain, a concept defeated in the 17 century, after anatomical studies demonstrated that there was no communication between the brain and nasal fossa4. From the end of 19 century on, various studies have demonstrated the association between nasal and pulmonary diseases. Kratchmer (1870) demonstrated an increase in resistance of lower airways in cats when the nostrils were stimulated with irritating factors, such as sulfur dioxide and cigarette smoke. Voltolini (1871) reported a case of asthma improvement after the patient was submitted to nasal polypectomy13. Many studies demonstrated an improvement in asthmatic symptoms in patients submitted to nasal surgeries, whereas other authors obtained negative results, showing the controversy3,9. One of the explications is that the improvement in treatments to control asthma and better understanding of the disease would be responsible for the results obtained4.
The proposed mechanisms to explain this relation between the lower and upper airways are: nasal-bronchial reflex originated in the nose and paranasal sinuses; retronasal secretion of infected pr inflammatory material; release of inflammatory mediators through paranasal sinuses; oral breathing; reduction of beta-agonists by sinusal infection; and sinusal secretions stimulating extrathoracic receptors6.
Data from the National Health Survey indicated that sinusitis is present in 14.7% and asthma in 5.14% of the population in the United States, resulting in absenteeism and an impact on economy of 6.2 billion dollars11,12. Chronic sinusitis coexists in 40 to 75% of the patients with asthma.
The objective of the present study was to evaluate retrospectively the results of endoscopic sinus surgery when treating patients with asthma who also had chronic rhinosinusitis and observe the effects on pulmonary status.
MATERIAL AND METHODWe conducted a retrospective study based on the medical files of patients submitted to endoscopic sinus surgery for chronic rhinosinusitis between 1996 and 1999, at the Discipline of Otorhinolaryngology at Hospital das Clínicas da Faculdade de Medicina, USP. Patients who had asthma in the medical history were selected, amounting to 53 patients. Out of this total, 13 (24.5%), were not properly followed-up post surgically; therefore, we excluded them from the study. The remaining 40 patients were, analyzed according to age, sex, underlying disease, personal history, treatments conducted, and asthma after surgery. Patients answered questionnaires scoring the symptoms from 1 (better) to 10 (worse), and we considered improvement if patients had a reduction in score of at least 5 points.
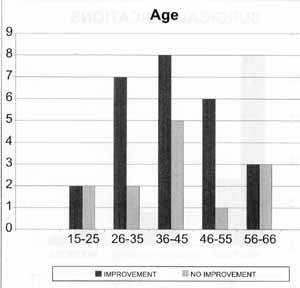
Graph 1. Distribution of patients according to age.
Among 40 studied patients, 30 (75%), were women and 10 (25%), were men, in a 3:1 proportion. Ages ranged from 15 to 66 years, mean age of 41 years (Graph 1). Thirty one patients (77.5%) had associated nasal polyposis, and 23 (74.2%) had improvement of pulmonary symptoms after surgery; 6 patients (15%) had chronic sinusitis and 2 of them (33%) had improvement of asthmatic symptoms; 3 patients (7.5%) were operated of mucocele and 2 (66.6%) improved their pulmonary symptoms (Graph 2). As to history, 15 patients (37.5%) had rhinitis, and 10 of them (66.6%) improved asthma after the surgery; 3 patients (7.5%) had intolerance to acetyl salicylic acid and they all improved after the surgery (Graph 3). All patients had been submitted to endoscopic sinus surgery and in some cases there was associated external approach of maxillary or frontal sinuses. In general, 27 patients (67.5%) experienced improvement of asthma after the surgery. There was no improvement in 13 cases (32.5%), but no patients reported worsening of symptoms after surgery (Graph 4).
DISCUSSIONThe association between nasal sinusal disease and asthma has been widely discussed by many authors1, however, there is no unquestionable pathophysiological model that demonstrates the association of these two diseases. Although there is no direct cause-effect relation between treatment of nasal sinusal disease and improvement of asthma, a large percentage of patients benefits from surgical treatment6,10. Our data showed improvement in asthmatic condition in 27 patients (67.5%), and 18 of them (45.5%) had a significant improvement after endoscopic sinus surgery (more than 7 points in the score).
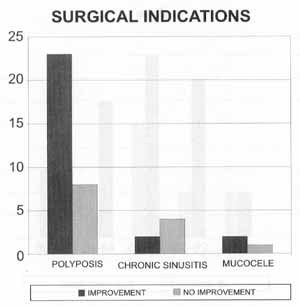
Graph 2. Distribution of patients according to surgical indications:
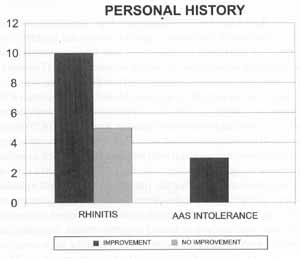
Graph 3. Distribution of patient according to personal history.
According to Senior et al., incidence of rhinitis in asthmatic patients is 80%, whereas 5% to 15% of patients with perennial rhinitis have asthma and 53% to 75% of children with asthma have alteration in the radiological exam of paranasal sinuses12. In our study, we found an incidence smaller than in the literature, amounting to 15 patients (37.5%) with rhinitis associated with asthma. It is important to keep in mind that in our study only asthmatic patients who had nasal surgical indications were included, which may account for the difference.
The relation between asthma and nasal polyp was analyzed by Larsen et al., showing that 7% to 15% of patients with asthma had nasal polyp, and the highest incidence was among patients who were older than 50 years7. Various surgical techniques are adopted according to the nasal sinusal disease diagnosed and the experience of the surgeon. English (1986), studied 205 asthmatic patients dependent on steroids and had symptom improvement in 40% of them after endonasal polypectomy12. Stammberger reported a study of 54 patients with asthma and chronic sinusitis who underwent functional endoscopic sinus surgery and had a subjective improvement of pulmonary symptomsin 83% of the cases, confirmed through pulmonary function tests12.
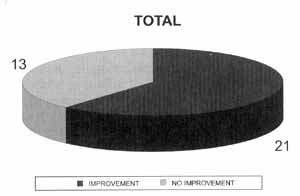
Graph 4. Distribution of patients according to progression of case.
According to Senior et al.13, improvement of asthmatic symptoms is still present years after the surgery. Kennedy et al. observed that 36 (86%) patients had improvement whereas 3 patients (7.1%) did not experience changes in the condition and 3 (7.1%) had worsening of symptoms. As to use of corticoids, out of a total of 24 patients who used the medication, 19 managed to reduce the dose, 3 maintained the same doses and 2 patients needed increased doses after endoscopic surgery12. Dunlop et al. found 40% improvement resulting in reduction of use of corticoids and 6% worsening of asthma symptoms after endoscopic sinus surgery12. The study by Nishioka et al. showed an improvement in, asthma in 80% of the patients2. Our data demonstrated improvement of asthma condition in 74.2% of patients with polyposis submitted to endoscopic sinus and nasal surgery. None of the patients who underwent surgery showed worsening of asthmatic symptoms.
Many studies showed that there is a reduction of asthma symptoms with nasal surgery; however, none of them had statistically significant data through pulmonary function tests1. Studies by Nakamura, Ikeda, and Stammberger, showed significant improvement detected through these tests. There was no correlation between severity of chronic sinusitis and results of pulmonary function tests, both for pre and post-operative tests1,10. Patients who had more improvement of nasal symptoms did not necessarily have improvement in control of asthma; however, the ones who had worsening of nasal symptoms also experienced poor pulmonary results6. There is no difference between patients with or without polyposis2. Control of patients with nasal polyp and sinusal disease shows worse results in asthmatic patients, and it is still more evident when associated with intolerance to acetyl salicylic acid In such patients, there were no differences between those submitted to endoscopic surgery and the others submitted to external approach7,10. Our sample showed that all patients with intolerance to acetyl salicylic acid had improvement of asthmatic condition. Since many analgesic and anti-inflammatory medications may induce to severe asthma episodes, and many patients with Widal's triad (asthma, nasal polyposis and intolerance to AAS), initially present only nasal symptoms, otorhinolaryngologists should be careful when prescribing such drugs to patients.
CONCLUSIONEndoscopic sinus surgery in patients with chronic rhinosinusitis refractory to clinical treatment resulted in improvement of asthmatic condition in a significant number of patients. It suggests a correlation between the two diseases, and we should always consider the possibility of surgical intervention in treating rhinosinusitis refractory to clinical treatment in patients with asthma. It is important to bear in mind that none of the studies indicated the performance of nasal surgery for control of asthma, unless it was associated with chronic rhinosinusitis refractory to concomitant clinical treatment13.
REFERENCES1. DINIS, P. B.; GOMES, A. - Sinusitis and Asthma: How Do They Interrelate In Sinus Surgery? American Journal of Rhinology, 11(6): 421-8, 1997.
2. DUNLOP, G.; SCADDING, G. K.; LUMD, V. J. - The Effect of Endoscopic Sinus Surgery on Asthma: Management of Patients with Chronic Rhinosinusitis, Nasal Polyposis, and Asthma. American Journal of Rhinology, 13(4): 265, 1999.
3. FRIEDMAN, W. H.; KATSATONIS, G. P.; SLAVIN, R. G.; KANNEL, P.; LINFORD, P. - Sphenoethmoidectomy: its role in the asmathic patient. Otolaryngology Head and Neck Surgery, 90 (2): 171-7, 1982.
4. GOLDSTEIN, M.F.; GRUNDFAST, S.K.; DUNSKY, E.H.; DVORIN, D j.; LESSER, R.- Effect of functional endoscopic sinus surgery on bronchial asthma outcomes. Arch. Otolaryngol. Head Neck Surg., 125: 314-319, Mar, 1999
5. GRANSTROM, G.; JACOBSSON, E.; JEPPSSON, P. H. - Influence of Allergy, Asthma and Hypertension on Nasal Polyposis. Acta Otolaryngology (Stockh), 492: 22-27, 1992.
6. IKEDA, K.; TANNO, N.; TAMURA, G.; SUZUKI,H.; OSHIMA,T.; SHIMOMURA, A; NAKABAYASHI,S.; TAKASAKA,T. - Ann. Otol. Rhinol. Laryngol., 108: 355-359, 1999
7. LARSEN, K. -The clinical relationship of nasal polyps to asthma. Allergy Asthma Proc., 17(5): 243-9, 1996.
8. LARSEN, K.; TOS, M. -Clinical Course of Patients with Primary Nasal Polyps. Acta Otolaryngology (Stockh), 114: 556-559, 1994.
9. MANNING, S. C.; WASSERMAN, R. L.; SILVER, R.; PHILLIPS, D. L. -Results of Endoscopic Sinus Surgery in Pediatric Patients with Chronic Sinusitis and Asthma. Arch. Otolaryngol. Head and Neck Surg., 120 (10): 1142-5, 1994.
10. NAKAMURA, H.; KAWASAKI, M.; HIGUCHI, Y.; TAKASHI, S. - Effects of Sinus Surgery on Asthma in Aspirin Triad Patients. Acta Otolaryngol. (Stockh), 119: 592-598, 1999.
11. PARK, A. H.; LAU, J.; STANKIEWICZ, J.; CHOW, J. - The Role of Functional Endoscopic Sinus Surgery in Asthmatic Patients. The Journal of Otolaryngology, 27(5): 275-80, 1998.
12. SENIOR, B. A.; KENNEDY, D. W. -Management of sinusitis in the asthmatic patient. Annals of Allergy, Asthma, & Immunology, 77 (1): 6-15, 1996.
13. SENIOR, B. A.; KENNEDY, D. W.; TANABODEEJ.; KROGER, H.; HASSAB M.; LANZA, D. C. -Long-term impact of functional endoscopic sinus surgery on asthma. Otolaryngol. Head Neck Surg.,121 (1):66-8, 1999.,
* Assistant Physician, Ph.D. of Clinical Otorhinolaryngology at Hospital das Clínicas da Faculdade de Medicina, Universidade de São Paulo (HC-FMUSP).
** Resident Physician of Clinical Otorhinolaryngology at HC-FMUSP.
*** Trainee Physician.
**** Associate Professor of the Discipline of Otorhinolaryngology FMUSP.
Study conducted at the division of Clinical Otorhinolaryngology, Hospital das Clínicas da FMUSP.
Address for correspondence: Fabrizio Ricci Romano - Divisão de Clínica Otorrinolaringológica - Hospital das Clínicas FMUSP.
Avenida Dr. Enéas de Carvalho Aguiar, 255 - 6° Andar - Sala 6021 - São Paulo/ SP - Fax: (55 11) 280-0299 - E-mail: ted80@uol.com.br
Article submitted on May 18, 2000. Article accepted on August 10, 2000.


