INTRODUCTIONAnatomical proximity of components of the ear and the temporomandibular joint (TMJ) almost always motivates patients with TMJ disorders to come to Otorhinolaryngologists.
The medical literature, however, helps very little with the clarification of diagnosis.
Within odonthologic scene, there is a trend of considering TMJ disorders as a set of nosologically different affections, which share common signs and symptoms.
TMJ is a real diarthrosis, bi-condylar, and the most complex in the human body8 for two reasons: it is the only one that allows rotation and translation movements because of the dual joint of the condyle, that is, the condyle articulates with the inferior surface of the disk and the posterior portion of articular eminentia articulates with the superior surface of the disk. In addition, there are two joints connected to one single bone, the mandible, that work simultaneously.
Muscles that are related to TMJ - temporalis, masseter and lateral and medial pterygoid - both move the mandible and are responsible for precise coordination of its staggering movements19, within the limitations determined by the ligaments. These ligaments guarantee the integrity and the limitation of the joint. If it is extended beyond its limits, the length of ligaments may be impaired. Ligaments are not capable of distending much - if this happens, they are elongated and suffer subluxation. This elongation causes changes in biomechanics and may generate specific pathologies.
Therefore, the source of pain in TMJ disorders may originate from the muscles, the ligaments or the fascia, represented by stretching, forced or maintained contraction, ischemia and hyperemia, as well as trauma and other inflammatory factors. Pain may be referred, if it stems from a mastication muscle in hyperactivity, or be located at the TMJ2.
As a response to pain, we may have a motor secondary effect, such as myospasm of tensor tympani muscle. This situation would lead to pull of the malleus and tympanic membrane and the consequent change of sound conduction through the middle ear, what would justify the complaint of subjective hearing loss and otalgia12,17,29.
The modern history of TMJ disorder started with the publication by otorhinolaryngologist Costen9 in 1936. He described a syndrome comprising the following symptoms: tinnitus, vertigo, articular pain, otalgia, hearing loss and ear fullness, relating the complaints to occlusion alterations, causing posterior sliding of condyle and consequent compression of nervous structures.
Sicher25 attributed the pain symptoms to spasms of mastication muscles, rejecting the hypothesis of compression of nervous structures by the condyle.
Carlsson5 reported that the posterior deviation of the condyle would cause tension and compression of tissues on the articulation area, generating impulses that would travel to the lateral vestibular nucleus, where axons from semicircular canals form their synapses, reaching other sensorial areas. Arlen1 believed that the symptoms related to otomandibular syndrome were justified by their embryonic origin - normal pattern would have been established within the brainstem and movement of mandible and ear ossicles had been integrated.
Various studies3,4,15,19 tried to confirm the existence of ENT symptoms triggered by muscle, articular or nervous alterations of TMJ but nothing was determined with certainty about etiological factors.
As we can see, after years of study following Costen9, etiological factors of TMJ disorder are still undefined. Integration with other health care professionals seems to be essential for confirming the hypotheses so far made.
This study aimed at carrying out an analysis with patients who had TMJ disorder associated to otological symptoms, in order to check main symptoms, type of associated pathologies and correlation with audiometric findings, if possible.
MATERIAL AND METHODThe sample consisted of 40 patients, both sex, referred randomly by the Service of Temporomandibular Disorders of Faculdade de Odontologia da Universidade Federal do Rio de Janeiro. Patients who had specific otorhinolaryngologic complaints were referred to clinical ENT and audiological assessments.
We excluded all patients who had history of chronic otitis, exposure to noise, tinnitus (present before TMJ dysfunction), occupational deafness or otological surgery.
All selected patients were assessed jointly by the team during a crisis of pain, so that diagnosis could be defined using the criteria by Bell2 for interpretation of complaint, anamnesis and physical exam.
Later, we conducted otoscopy to exclude cerumen build-up and patients were referred to audiometric exam at HUCFF.
We conducted a descriptive analysis of clinical data, frequency of sex, frequency of TMJ disorder, frequency of age range and audiometry, relation between symptoms and odonthological diagnosis and the relation between symptoms and audiometric exam. After determining the frequency of TMJ disorder, we conducted statistical analysis of data, checking the relation and significance of odonthological diagnosis and audiometric alterations.
Statistical analysis was based on t test of Student for independent samples, in order to check if there was significant age difference between the two groups. To compare proportions, we applied qui-square test or exact test of Fisher. The criteria for significance were 5%.
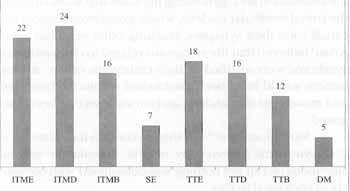
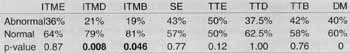
Figure 1. Frequencies of temporomandibular disorders.
ITME = Left TM ligament attachment; ITMD = Right TM ligament attachment; ITMB = Bilateral TM ligament attachment; SE = Ernest Syndrome; TTE = Left temporal tendinitis; TTD = Right temporal tendinitis; TTB = Bilateral temporal tendinitis; DM = Miofacial dysfunction.
Female patients were more frequent (92.5%) than male patients (7.5%).
The most common TMJ disorder was pain on the point of attachment of right temporomandibular ligament (ITMD) (Fig. 1).
The mean age of the 40 patients was 41.1 years, standard deviation (SD) of 15.8, varying from 16 to 73 years.
At audiometric assessment, 62.5% of the exams were normal, whereas 37.5%, were abnormal. We observed statistically significant difference (p = 0.0007) in the average between patients with abnormal and normal audiometry, that is, patients with abnormal audiometry were in average older than patients with normal audiometry (Table 1).
In a questionnaire, we listed the most frequent otorhinolaryngologic symptoms: right otalgia (72.5%), left otalgia (77.5%), bilateral otalgia (52.5%), hearing loss (15%), ear fullness (17.5%), tinnitus (17.5%) and autophony (15%).
Fig. 2 presents the percentage of assessed symptoms.
Table 2 associates types of TMJ disorders with otalgia showing the significant association between them. The attachment of left temporomandibular ligament (ITME) was the disorder that had most otalgia (95%) and it was statistically significant (p = 0.003). We also noticed a slight tendency of patients with disorder in the bilateral attachment of temporomandibular ligament (ITMB) to have otalgia (p = 0.003).
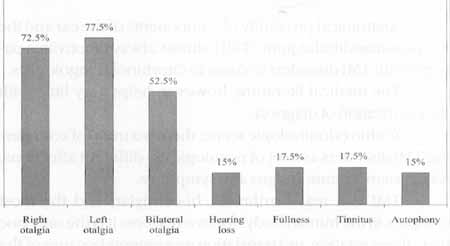
Figure2. Frequency of most common ENT symptoms reported by patients.
TABLE 1 - Frequency of normal and abnormal audiometry compared to mean age of patients.
The correlation of TMJ disorder with audiometric curve alterations was not significant - due to low incidence of some disorders no statistical analysis could be conducted (Table 3). Values of Table 3 varied according to the number of cases that presented these disorders: they could be isolated or associated, showing a greater percentage of alteration, but only two of them were significant: ITMD and ITMB.
DISCUSSIONAs previously mentioned, we proceeded with the analysis of complaint, anamnesis and physical exam. The most commonly found disorder (Graph 1) was related to painful points represented by temporal tendinitis in the attachments of temporomandibular ligaments, followed by syndrome of Ernest28 (which included a painful point in the attachment of stylomandibular ligament) and miofacial dysfunction, both characterized by trigger points27.
Gross14, in studies showing the importance of the physical exam in patients with temporomandibular disorder and using palpation, found that lateral pterygoid muscle was the most altered, followed by masseter and temporalis muscles.
None of the other references researched followed-up temporomandibular disorders as we proposed. In our sample, the most common source of pain was ITMD, with 24 patients. Due to lack of comparative data, we did not discuss independently the correlation of each disorder; but we preferred to follow the literature and discuss them as a whole.
TABLE 2 - Correlation between type of temporomandibular disorder and symptom: left (OE), right (OD) and bilateral (OB) otalgia.
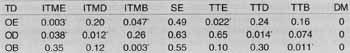
ITME = Left TM ligament attachment; ITMD = Right TM ligament attachment; ITMB = Bilateral TM ligament attachment; SE = Ernest Syndrome; TTE = Left temporal tendinitis; TTD = Right temporal tendinitis; TTB = Bilateral temporal tendinitis; DM = Miofacial dysfunction; (*) significance level of 5%.
TABLE 3 - Correlation between temporomandibular disorders and audiometric curve (abnormal or normal).
ITME = Left TM ligament attachment ITMD = Right TM ligament attachment; 1TMB = Bilateral TM ligament attachment; SE = Ernest Syndrome; TTE = Left temporal tendinitis; TTD = Right temporal tendinitis; TTB = Bilateral temporal tendinitis; DM = Miofacial dysfunction.
As to sex distribution, our findings were in accordance with the literature. Bush4, Garcia11, Giordani13, Koskinen16 and Paiva2l showed incidence in female higher than in male patients. It should probably be due to higher absorption of emotional stress in women7, resulting in lowering of physiological tolerance level and increase of muscle hyperactivity, leading, to functional imbalance. Alternatively, Rubstein24 showed a higher prevalence in men.
Regarding age, the average age was 41.1 years, ranging from 16 years to 73 years. Most of the patients were within the third and fourth decades of life, and the mean age was in accordance with the literature4, 16. The imbalance would be due to functional overload or parafunctional activity (sleep position, trauma and bite, among others) developed by the subject, what could lead to inflammatory process in tissues and muscles2,3.
As to audiometric assessment, there was prevalence of normal results (62.5%) compared to abnormal ones (37.5%). In the 15 exams we detected abnormal results, the most common finding was sensorineural hearing .loss. Twelve patients had mild to severe unilateral or bilateral loss and mean age of 51.7 years. There were two other patients with mixed hearing loss and one case of conductive loss. We detected statistically significant differences among patients with abnormal audiometry because their mean age was higher than the mean age of patients with normal audiometry (Table 1).
Our data were compatible to those of Bernstein3 et al., who believed that the sensorineural loss detected by them was due to presbyacusis, that is, the patient had already had the lesion. That assumption contradicted the studies by Pinto23, who advocated the theory of disk-maleolar ligament - later on confirmed by Ioannides and Hoogland15, after dissection in cadavers, to justify the hearing loss presented by patients. Anterior displacement of maleolar disk, if not firmly attached to tympanic fissure wall, would pull the malleus and lead to alteration of the ossicle chain and, consequently, subjective hearing loss - this fact, according to Eckerdal10, would not take place in live people, because the ligament is attached to the walls of the fissure.
Koskinen et al.16 and Toller26, on the other hand, did not detect significant audiometric alterations in patients with and without TMJ disorder.
We did not detect the significance we expected when analyzing otological symptoms and most frequent TMJ disorder separately.
In our sample, otalgia was undoubtedly the most evident symptom, unilateral or bilateral, followed by fullness in the ear, tinnitus, hearing loss and autophony (Graph 2) - compatible with different authors3,4,8,9,15.
Otalgia may originate locally20, or be secondary to other causes that lead to referred pain2,16. It is possible that inflammatory exsudate reaches middle ear and causes local alterations by means of permeability of petrotympanic fissure18. Chole6, supported by the studies of Ciancaglini7 , believed that the existence of otalgia could be explained by the anatomical proximity of middle ear and temporomandibular joint structures. Patients who have neuromuscular malocclusion may develop an accommodation of the free space of the joint, requiring more muscle tone to correct the posture. This would be due to muscular-mastication disorders that would lead to spasms and, consequently, pain8,12.
Parker and Chole22 did not explain the cause of tinnitus and vertigo in patients who had TMJ disorder: they confirmed that future studies would lead to a definite solution. In studies carried out with 28-day embryos Arlen' tried to show that the phylogenetic origin of the same blastema would be the origin of normally found otological signs and symptoms.
Our study is in accordance with the literature when it addressed signs and symptoms, confirmed by statistically significant differences in some cases. However, despite the fact that patients presented evident symptomatology, it was not possible to correlate it with the definite data that would confirm the existing pathophysiology.
CONCLUSIONBased on the selected sample of patients with temporomandibular disorders we concluded that:
1. the frequency is higher in female subjects (92.5%), aged between the 3rd and 4th decades of life;
2. otalgia was the main complaint (77.5%);
3. the most common source of pain was the right attachment of temporomandibular ligament;
4. audiometric assessment enabled the analysis of two different groups: first, a group of normal audiometry (62.5%) with mean age of 35.2 years; and a second group of patients with abnormal audiometry (37.5%) and mean age of 51.7 years. Both groups had median duration of ENT symptoms of 24 months.
The authors would like to acknowledge the financial support provided by Capes.
REFERENCES1. ARLEN, H. - Otolaryngologic manifestations of craniomandibular disorders. Dent. Clin. North Am., 27(3): 523 - 526, 1983.
2. BELL, W. E. - Dores orofaciais.- Classificação, diagnóstico, tratamento. 1ª edição, Rio de Janeiro, Quintessence Books, 1991.
3. BERNSTEIN, J. M.; MOLL, A. N. & SPILLER, H. - Temporomandibular joint dysfunction masquerading as disease of the ear, nose and throat. Trans. Acad. Ophtalmo. Otology, 73:1208-1217, 1969.
4. BUSH, F. M. - Tinnitus and otalgia in temporomandibular disorders. J. Prosthet Dent, 58(4): 495-498, 1987.
5. CARLSSON, S. D. -A possible explanation of dizziness in Costen syndrome. Am. J. Orthod. Dentofacial Orthop., 41:470 - 473, 1955.
6. CHOLE, R. A. & PARKER, W. S. -Tinnitus and vertigo in patients with temporomandibular disorder. Arch. Otolaryngol Head Neck Surg., 118(8): 817-821, 1992.
7. CIANCAGLINI, R.; LORETI, P. & RADAELLI, G. -Ear, nose and throat symptoms in patients with TMD: The association of symptoms according to severity of arthropathy. J Orofacial Pain, 8(3): 293-297, 1994.
8. COOPER, B. C. & COOPER, D. L. - Recognizing otolaryngologic symptoms in patients with temporomandibular disorders. J. Craniomand. Pr., 11 (4): 260-267, 1993.
9. COSTEN, J. B. - Neuralgia and ear symptoms associated with disturbed function of the T.MJ. J. Am. Med. Assoc., 107: 252-254, 1.936.
10. ECKERDAL, O. - The petrotympanic fissure: a link connecting the tympanic cavity and the temporomandibular joint. Cranio, 9(1):15-22, 1991.
11. GARCIA, A. R.; MADEIRA, C. M. & MONTEIRO, A. R. - Sintomas otológicos nas disfunções temporo-mandibulares: etiologia, diagn6stico a tratamento. ATM Scientia, vol 1, 1997.
12. GELB, H.; CALDERONE, J. P.; GROSS, S. M. & KANTOR, M. E. -The role of the dentist and the otolaryngologist in evaluating temporomandibular joint syndromes. J Prosthet Dent., 18(5): 497-502, 1967.
13. GIORDANI, A. & ADOBIO, K. A. - Placa estabilizadora de Michigan: a sensação de zumbido. Rev. Assoc. Paul. Cir. Dent., 49(5): 1995.
14. GROSS, A. & GALE, E. N. - A prevalence study of the clinical signs associated with mandibular dysfunction. J. Am. Dent Assoc, 107: 932-936, 1983.
15. IOANNIDES, C. A. & HOOGLAND, G. A. - The disco-maleolar ligament a possible cause of subjective hearing loss in patients with temporomandibular joint dysfunction. J. Cranio-maxillofac Surg, 11(5): 227-231, 1983.
16. KOSKINENJ; PAAVOLAINEN, M.; RAIVIO, M.& ROSCHIER, J. - Otological manifestations in temporomandibular joint dysfunction. J. Oral Rehabil., 7: 249-254, 1980.
17. KREISBERG, WK. & TURNER, J. - Dental causes of referred otalgia. Ear Nose Throat J, 66: 30-48, 1987.
18. MARASA, F. K. & HAM, B. D. - Case reports involving the treatment of children with chronic otitis media with effusion via craniomandibular methods. Cranio. 6(3):256-270. 1988.
19. MONGINI, F. -, ATM a musculos craniocervicofaciais: fisiopatologia a tratamento. Sao Paulo, Ed Santos, 1997.
20. MURTAGH, J. -The painful ear. Aust Fam Physician, 20(12): 1774-1784, 1991.
21. PAIVA, G.; NASK, M. K.; PAIVA, A. F.; ROSSI, S. S. B. & PAIVA, P. F. - Características de pacientes portadores de desordem temporo-mandibular: avaliação de 400 casos. ATM Scientia, vol 1, 1997.
22. PARKER, W. S. & CHOLE, R. A. - Tinnitus, vertigo and temporomandibular disorders. Am J Ortbod Dentofacial Orthop, 107(2): 153-158, 1995.
23. PINTO, O. F. - A new structure related to the temporomandibular joint and middle ear. J Prosthet Dent Jan Feb, 12(1):95-103, 1962.
24. RUBINSTEIN, B.; AXELSSON, A. & CARSSON, G.E. Prevalence of sins and symptoms of craniomandibular disorders in tinnitus patients. J. Craniomand Disorders: Facial & Oral Pain, 4(3): 186-192, 1990.
25. SICHER, H, -Temporomandibular articulation in mandibular overclosure. J. Am. Dent. Assoc., 36: 131 - 139, 1948.
26. TOLLER, M. O & JUNIPER, R. P. - Audiological evaluation of the aural symptoms in temporomandibular joint dysfunction. J. Cranio-maxillo fac Surg., 21: 2-8, 1993.
27. VERNON, J.; GRIEST, S. & PRESS, L. - Attributes of tinnitus that may predict temporomandibular joint dysfunction. J. Craniomand Pract, 10(4): 282-289, 1992.
28. VINCENT, M.; AMADO, S. M.; FACANHA, A. & NOVIS, S. Síndrome de Ernest, experiência de 76 casos de revisão de diagnóstico diferencial. Cefaléia e dor, 1(1): 21-27, 1996.
29. YOUNISS, S. -The relationships between craniomandibular disorders and otitis media in children. Cranio, 9(2):169-173, 1991.
* Master Degree in Otorhinolaryngology, Faculdade de Medicina da Universidade Federal do Rio de Janeiro (UFRJ).
** Faculty Professor of the Discipline of Otorhinolaryngology, FM - UFRJ.
*** Joint Professor of the Department of Dental Prosthesis and Materials of the School of Odonthology, UFRJ.
**** Mater Degree under way at the Post-Graduation Course in Otorhinolaryngology, FM- UFRJ.
***** Joint Professor of the Discipline of Otorhinolaryngology, FM - UFRJ.
Summary of Master Dissertation approved in May 1998. Carried out in the Service of Otorhinolaryngology at Hospital Universitário Clementino Fraga Filho (HUCFF) and at the Ambulatory of Temporomandibular Disorders at Faculdade de Odontologia - UFRJ.
Study presented as Poster at 34° Congresso Brasileiro de Otorrinolaringologia, November 18 - 22, held in Porto Alegre /RS.
Address for correspondence: Serviço de otorrinolaringologia - HUCFF (Secretaria) - Av. Brigadeiro Trompowski, s/ n°, 11° andar - Tel: (55 21) 562-2842.
Ilha do Fundão - Rio de Janeiro/ RJ.
Article submitted on August 13, 1999. Article accepted on June 9, 2000.


