INTRODUCTIONThe symptom of nasal obstruction is a common inducement for a patient to seek professional help and the usefulness of current methods of objective assessment of nasal patency is discussed in the following brief review.
Why:
In many cases, a careful history and examination enable a diagnosis of the complaint o£ nasal obstruction to be made and appropriate treatment to be instituted.
However, nasally obstructed pediatric patients seldom complain of the symptom and there are adult patients in whom the symptom can be misleading to both patient and practitioner.
In patients whose diagnosis is uncertain supporting evidence by objective testing can be useful in confirming or refuting an initial clinical impression. Indeed, it is not unusual for the symptom of nasal obstruction to be unexplained and objective methods can be helpful in establishing a diagnosis and avoiding inappropriate treatment. In addition to diagnostic aids, objective methods are also of particular value (see below) for monitoring therapy, for medicolegal documentation, for allergy challenge and drug assessment and for research.
Although some patients may recognize the presence of unilateral nasal obstruction, subjective assessment of the degree of nasal patency is unreliable and correlation with rhinoscopic or objective findings is weak1-6. Indeed, subjects are usually unaware of major physiological changes in nasal patency that occur in healthy noses in response to posture, to exercise and to the spontaneous nasal cycle. Moreover, the chance finding of obvious obstruction in uncomplaining patients is not unusual nor is it unusual for complaints of obstruction to be unaccompanied by confirmatory findings.
The sensation of the degree of nasal patency can be altered not only by pathology but also by exposures to ambient conditions. For example, inspiratory airflow stimulates thermal receptora and the sensation of chill increases with thermal demands. Thermal demands depend on the magnitudes of flow, temperature and humidity of inspiratory air. Cold, dry air and deep breaths increase the sensation of nasal patency.
Constituents of ambient air also can affect the sensation of nasal patency. Several aromatic substances that contain L-menthol stimulate thermal neurosensors amplify the sensation of airflow and patency7, 8. By contrast, second-hand tobacco smoke produces the opposite effect in many healthy subjects9. It is of interest to note that in neither of the latter two examples do objective tests demonstrate a change in nasal resistance to airflow.
Rhinoscopic findings too are subjective and assessments can differ even between skilled clinicians and they can differ also from objective measurements10, 11.
An important limitation of rhinoscopy, especially in the leptorrhine Caucasian nose, is concerned with the constricted dimensions of the nasal valve. This narrow segment is the commonest site of nasal obstruction by structural and/or mucosa} abnormality but introduction of a speculum is invasive since it alters tissue relationships in this critical region. A minor displacement of either wall of the nasal valve by as little as 1 mm is not easy to detect by visual inspection. Yet, since resistance to airflow is related exponentially to cross-sectional area of a conduit, it can cause a major change in objective measurements of airflow resistance1, 12, 13. Thus rhinomanometry is a sensitive indicator of small dimensional changes in nasal cross-sectional area that can be detected also by non-invasive acoustic rhinometry and yet can easily escape detection or accurate assessment by rhinoscopy.
When:
In view of the limitations of traditional methods and criteria and their subjective basis there are many cases in which objective techniques can be helpful in assessment of nasal patency. In addition to their use in cases where a confident diagnosis cannot be made, objective methods are of great value for monitoring therapy14-18. The benefits of any one of an ever increasing number of therapeutic modalities and medications available for nasal treatment are easier to assess and record if objective criteria are employed. favorable response may be ascertained objectively before either patient or practitioner is aware and may thus warrant continuation of current therapy. Similarly, useless or unfavorable therapy can be abandoned at an early stage and avoided for future use.
Records of objective findings can be of great value when practitioners employ measures that risk patient dissatisfaction and in cases of nasal trauma, each can assume medicolegal importance. An objective record is useful also for comparison when a patient returns after an extended period of time. It is increasingly common for health insurance providers to require rhinomanometric confirmation of a diagnosis before their agreement to accept financial responsibility for therapy.
In addition to their clinical applications objective measures are widely used in laboratory investigations and research of nasal diseases, new medications, environmental and industrial exposures and also in studies of the nose itself and its effects on other body functions19.
Figure 1. Rhinomanometric recording of transnasal pressure against flow during breathing at rest through an unremarkable nose and through an obstructed nose.
HOW
Two main methods are in current use for objective assessment of nasal patency throughout the world. An aerodynamic measurement of nasal airflow by rhinomanometry and a geometric measurement of the nasal airway by acoustic rhinometry.
Rhinomanometry
The International Committee on Objective Assessment of the Nasal Airway, formerly named the International Committee on Standardization of Rhinomanometry20 recommends that nasal patency be described in terms of resistance to respiratory airflow as the ratio between concomitant measurements of transnasal flow and pressure (Rn=DP/V ) in SI units of Pa/cm3/sec.
Recording of transnasal pressure against flow during nasal breathing produces a sigmoid tracing (Figure 1) and the ratio between rectangular coordinates (DP/V) defines resistance at any chosen point or points on the curve. Choice of a suitable point differs between centers, (a)100 Pa, (b) 150 Pa and (c) peak values are common choices. As a useful alternative, computation of digitized signals enables (d) average resistances and several other respiratory variables to be determined. The resistance values obtained by methods (a), (c) and (d) are similar over a range extending well beyond normal and (b)150 Pa values are about 25% greater.
Transnasal pressures are determined by 3 common methods:
(1). Through a peroral tube to the oropharynx.
With lips closed around the tube the subject breathes through the nose and pressures between nostrils and oropharynx can be recorded. This method is termed posterior rhinomanometry.
(2). Through a fine tube sealed in a nasal vestibule.
The subject breathes through the unoccluded nasal cavity and postnasal pressures are conducted through the occluded side to the pressure recording tube. This method is termed anterior rhinomanometry.
(3). Through a fine tube inserted pernasally to the nasopharynx. This method is termed pernasal rhinomanometry.
Each method has advantages and disadvantages.

Figure 2. Toronto head-out displaccinent-type body plethysmograph
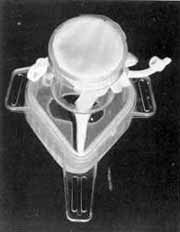
Figure 3. Modified CPAP mask with 400 mesh dacron resistor as a laminar flow element
Posterior rhinomanometry (1) includes adenoid tissue in the measured airway and is therefore particularly useful for pediatric measurements. Success requires patience and persistence of patient and observer and an experienced technician is almost invariably successful.
Anterior rhinomanometry (2) requires minimal cooperation by the subject. Adenoid obstruction of the respiratory airway cannot be determined by this method.
Pernasal rhinomanometry (3) requires minimal cooperation and is more expeditious than the anterior method.
In our own laboratories we use the Pernasal method (3) for adults19 and the post nasal method (1) for childrenz21. In both situations the measurements are made by experienced techinicians and failures are rare.
Transnasal airflow is measured also by 3 main methods in which airflow is directed through a flow measuring device (pneumotach):
(1) Via a nozzle inserted in a nasal vestibule as the opposite side is occluded.
(2) Via an open port of a facemask.
(3) With a head-out body plethysmograph.
As with Pressure measurements each method has advantages and disadvantages. Nozzles must be chosen and inserted with exceptional care since they risk distortion of the nasal valve with consequent exponential aerodynamic effects. Facemasks are not without hazard since the pressures exerted against facial tissues in order to obtain a seal, although remote from the nostrils, can affect the dimensions of the nasal portal22. We have given up use of SCUBA masks, and prefer modified CPAP masks or aviator/fireman type masks.
In our clinical laboratories we use a plethysmograph which caves the face entirely free14 (Figure 2). For field work or sleep studies we find a facemask more convenient. In each case airflow is directed through a pneumotach consisting of a resistor (cg fine mesh) which enables pressure differences between sides to indicate flow (Figure. 3).
Pressure and flow are transduced to electrical signals that are digitized and processed electronically to provide resistance measurements of the. nasal airway. The convenience of computerization that simplifies data acquisition, storage and manipulation is increasingly popular.
Acoustic rhinometry
Acoustic rhinometry is a relatively new technique that enables precise determination of cross-sectional area and volume of any nasal segment between nostril anel choana to be made23-25. It has a well established position in rhinological research since it can provide consecutiva measurements of nasal geometry in a rapid, reliable and non-invasive manner (eg nasal challenge, drug testing, nasal cycle) 26-29. In many centers the technique is used for clinical assessments before and after interventions (cg turbinectomy, scptoplasty, rhinoplasty)17, 30.
The technique offers particular advantages in accurate dimensional evaluation of the nasal valve region and the structural and mucovascular components of nasal obstruction25. The International Committee on Objective Assessment of the Nasal Airway is newly named to include acoustic rhinometry and the technique occupied much of the agenda for discussion at the European Rhinological Society Meeting in Copenhagen in june 1994. Standardization recomendations are in preparation that will enable proper comparison of results to be made between centers.
The method is based on analysis of reflected sound waves from the nasal cavities and although there are different systems available for data acquisition, the graphical patterns of nasal cavity geometry reported from different centers show close agreement25, 30, 31. In general, a sound-wave signal is generated from an electric spark or of longer duration from a loud-speaker.
Figure 4. Diagram of the Acoustic rhinometry system. (Reproduced with permission from Roithmann, R. et al., Acoustic rhinometry in the evaluation of nasal obstruction. Laryngoscope, 1994, in press).
Wave tubes (dimensions vary between centers) conduct the sound to a nasal cavity. Incident and reflected sounds are detected by a microphone and the signals are conducted to a progammed computer with a monitor display of computed values of cross-sectional areas, volumes and an area-distance graph. There are important differences between nasal adapters which connect the wave tube to the nostrils: Great tare must be exercised in choice and application of the adapter in order to avoid distortion of the compliant anterior nose and nasal valve which is the main site of both physiological and pathological nasal resistancezs12, 32. Figure 4 illustrates the Eccovison Acoustic Rhinometer system (Hood Laboratories, Pembroke, MA) we use in our Toronto laboratories which employs the following important recommendations:
1) in place of a nozzle which risks dilation of the nasal valve we use of a non-invasive nasal adapter (Figure 5). It is positioned to barely touch the margins of the nostril and water soluble lubricant jell expressed from a small syringe seals the junction and completes the acoustic coupling essential for rhinometric measurement. The expanded upper surfaces (about10x15 mm) of left and right adapters are obliquely molded to simplify close approximation with the margins of each nostril. A selection of sizes is available.
2) the subjects head is stabilized by a chin support. This minimizes change of head position that could distort the compliant nasal vestibule by pressure against the adapter attached to the wave tube which is clamped in position (Figure 5).
3) the stabilized head position also minimizes alteration of the angle of incidence and emergence of the acoustic signals during each series of tests.
4) four area-distance graphs with computations in good agreement (coefficient of variation < 5%)complete the series for 1 side and a similar procedure is performed on the opposite side.
In a clinical situation the left and right procedures are repeated following application of a topical decongestant (xylometazoline hydrochloride 0.1%) to determine the vascular constituem of mucosal volume and thus to enable the clinician to differentiate mucosal from structural componente of nasal obstruction (Figure 6).

Figure 5. Patient in position and stabilized for acoustic rhinometry data acquisition. (1) chin rest (2) non-invasive nasal adapter, (3) wave tube. (Reproduced with permission from Roithmann, R. et al., Acoustic rhinometry in the evaluation of nasal obstruction. Laryngoscope, 1994, in Press).
Figure 6. Acoustic rhinometry print-outs: (1) normal curve before and after topical decongestion of the nasal mucosa. Entrance of the nasal valve (curved arrow), anterior end of the inferior turbinate at the piriform aperture (arrow) ; (2) nasal polyp (curved arrow); (3) mucosal congestion. Note the significant increase in nasal cross-sectional area after topical decongestion of the nasal mucosa (arrow) ; (4) structural obstruction: anterior septal deviation. Topical decongestion of the nasal mucosa did not increase signiftcantly the minimal cross-sectional area (curved arrow). (Reproduced with permission from Cole, P., Roithmann, R. Rhinomanometry: clinical applications. In Diseases of the Sinuses: A comprehensive textbook of diagnosis and treatment. Gershwin, M.E., Incaudo, G., eds. Humana Press, 1994, in Press).
In some cases, a spring-loaded external dilator (Breathe Right TM, CNS, Inc. Chanhassen, MN) that, by adhesion to the skin overlying the compliant segment of the anterior nose, dilates the vestibule is used to define the anatomy and function of the nasal valve which is most commonly obstructed as a complication of rhinoplasty .
ConclusionsThere are many situations, as discussed above, in which objective rhinological assessment is of value to both rescarcher and clinician. Current technology has made available two main methods, acoustic rhinometry and computer-aided rhinomanometry.
Acoustic rhinometry is a static test that is independent from nasal airflow. It provides a rapid, minimally invasive and precise assessment of nasal geometry. Volume of mucovascular swclling can be quantified expeditiously in a manner that is particularly useful for measurements of rapidly changing airway dimensions as with nasal challenge tests. Precise measurements of nasal valve dimensions pre and post intervention can be obtained and recorded. The area-distance graph allows visualization of the site of obstruction.
Rhinomanometry is a dynamic test. It quantifies nasal breathing parameters and indicates how hard it is to breathe through the nose. The method enables mucovascular and structural components of nasal obstruction to be differentiated and quantified and the anterior, posterior or post-nasal (adenoid) site and severity of obstruction to be determined.
Either method can contribute substantially to appraisal of the nasal airway and together they provide a comprehensive picture of nasal airway structure and function.
REFERENCES1. Roithmann, R.; Cole, P.; Chapnik, J. et al.: A correlative study of acoustic rhinometry, rhinomanometry and the sensation of nasal patency. J Otolaryngol, 1994 (in press).
2. Naito,K.; Cole,P.; Fraschetti, J. et al.: Nasal patency: subjective and objective. Am J Rhinology, 3: 93-97, 1989.
3. Eccles, R.; Lancashire, B.; Tolley, N.S.; Experimental studies on nasal sensation of airflow. Acta Otolaryngol (Stock), 103: 303-306, 1987.
4. Jones, A.S.; Willatt, D.J.; Durham, L.M.; Nasal airflow: resistance and sensation. J Laryngol Otol, 103: 909-911, 1989.
5. Eccles, R.; Morris, S.; Tolley, N.S.; The effects of nasal anaesthesia upon nasal sensation of airflow. Acta Otolaryngol (Stockh), 106: 152-155, 1988.
6. McCaffrey, T.V.; Kern, E.B.; Clinical evaluation of nasal obstruction: a study of 1000 patients. Arch Otolaryngol, 105: 542-545,1979.
7. Burrow, A.; Eccles, R.; Jones, A.S.; The effects of camphor, cucalyptus and menthol vapour on nasal resistance to airflow and nasal sensation. Acta Otolaryngol (stock), 96: 157-161, 1983.
8. Eccles, R.; Griffiths, D.H.; Newton, C.G.; Tolley, N.S.; Effect of menthol isomers on nasal sensation of airflow. Clin Otolaryngol, 13: 25-29, 1988.
9. Urch, R.B.; Silverman, F.; Corey, P.; Shephard, R.J. et al.: Does suggestibility modify acure reactions to passive cigarette smoke exposure? Environ Res, 47: 34-47, 1988.
10. Hardcastle, P.F. et al.: Clinical or rhinometric assessment of the nasal airway: which is better? Clin Otolaryngol, 13: 381385,1988.of the nasal airway. Clin Otolaryngol, 10: 3-7, 1985.
12. Warren, D.W.; Hairfield, M.W.; Seaton, D.L.; Hinton, V.A.; The relationship between nasal airway cross-sectional area and nasal resistance. Am J Orthod Dentofac Orthop, 92: 390-395, 1987.
13. Chaban, R.; Cole, P., Naito, K.; Simulated septal deviations (2). Arch Otolaryngol Head Neck Surg, 114: 413-15, 1988.
14. Cole, P.; Roithmann, R. - Rhinomanometry: clinical applications- In: Gershwin M.E.; Incado G. - Diseases of the sinuses: acomprehensive textbook of diagnosisand treatment. Humana Press Inc., chapter 27, 1994 (in press).
15. Gordon, A.S.D.; McCaffrey, T.V.; Kern, E.B.; Pallanch, J.F.; Rhinomanometry for preoperative and postoperative assessment of nasal obstruction. Otolaryngol Head Neck Surg, 101: 20-26, 1989.
16. Berry, R.B.; Nasal resistance before and after rhinoplasty. B J Plastic Surg, 34: 105-111, 1981.
17. Grymer, L.F.; Illum, P.; Hilberg, O.; Septoplasty and compensatory inferior turbinate hypertrophy: a randomized study evaluated by acoustic rhinometry. J Laryngol and Otol, 107: 413-17, 1993.
18. Holmstrom, M.; Kumlien, J.; A clinical follow-up of septal surgery. Clin Otolaryngol, 13: 115-120, 1988.
19. Cole, P.; The respiratory role of the upper airways: a selective clinical and pathophysiological review. St. Louis, MO, 1-164,1993.
20. Clement, P.A.R.; Committee report on standardization of rhinomanometry. Rhinology, 22: 151-5, 1984.
21. Parker, L.P.; Crysdale, W.; Cole, P.; Woodside, D.G.; Rhinomanometry in children. Int J Paed Otorhinolaryngol, 17: 127-137, 1989.
22. Cole, P.; Havas, T.; Nasal resistance to respiratory airflow: a plethysmograph alternative to the face mask. Rhinology, 25: 159-66, 1987.
23. Hilberg, O.; Jackson, A.C.; Swift, D.L.; Pedersen, O.F.; Acoustic rhinometry: evaluation of nasal cavity geometry by acoustic reflection. J Appl Physiol, 43: 523-536, 1989.
24. Hilberg, O.; Jensen, F.T.; Pedersen, O.F.; Nasal airway geometry: comparison between acoustic reflections and magnetic resonance scanning. J Appl Physiol, 75: 2811-9, 1993.
25. Roithmann, R.; Cole, P.; Chapnik, J. et al.: Acoustic rhinometry in the evaluation of nasal obstruction. Laryngoscope, 1994 (in press).ckh), 113: 530-532, 1993.
27. Roithmann, R.; Shpirer, L; Chapnik, J. et al.: Acoustic rhinometry and the nasal provocation challenge in allergic patients. Am J Resp and Crit Care Med, 149 (part 2): A600, 1994.
28. Fisher, E.W.; Scadding, G.K.; Lund, V.J.; The role of acoustic rhinometry in studying the nasal cycle. Rhinology, 31: 57-61, 1993.
29. Fouke, J.M.; Jackson, A.C.; Acoustic rhinometry: effects of decongestants and posture on nasal patency. J Lab Cli Med, 9: 371-376, 1992.
30. Lenders, H.; Pirsig, W.; Diagnostic value of acoustic rhinometry: patients with allergic and vasomotor rhiniits compared with normal controls. Rhinology, 28: 5-16, 1990. 31. Grymer, L.F.; Hilberg, O.; Pedersen, O.; Rasmussen, T.R.; Acoustic rhinometry : values from adultswith subjective normal nasal patency. Rhinology, 29: 35-47, 1991.
32. Hirschberg, A.; Roithmann, R.; Parikb, S.; Cole, P.; The airflow resistance profile of healthy nasal cavities. Rhinology, 1994 (in press).
Trabalho realizado no Departamento de Otorrinolaringologia, Hospital Mount Sinai, Universidade de Toronto, Canada. Este projeto recebeu suporte da Saul A. Silverman Family Foundation e da Latner Family Trust/Dynacare, Toronto, Canada, como parte do Programa Internacional Canadense de Intercâmbio Científico em Otorrinolaringologia (CISEPO II) e da CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Ministério da Educação, Brasil.
* Clinical/research fellow, Departamento of Otorrinolaringologia, Mount Sinai Hospital, Toronto, Canada. Membro do Comitê Internacional de Avaliação Objetiva da Via Aérea Nasal.
** Professor de Otorrinolaringologia da Universidade de Toronto e Diretor de Pesquisa do Saul Silverman Nasal Airflow Laboratory and Clinical Investigation Unit, Mount Sinai Hospital, Toronto, Canada.
Endereço para correspondência: Dr. Renato Roithmann, Rua Felipe Camarco 408/304 - Porto Alegre-RS 90035-140 - Brasil
Artigo recebido em 09 de agosto de 1994.
Artigo aceito em 14 de dezembro de 1994.


